Cellulitis: What You Need to Know


What Is Cellulitis?
Cellulitis sounds a lot like cellulite, but the two conditions have nothing in common. Cellulite is dimpled skin caused by fatty deposits. Cellulitis is a painful skin infection that happens when bacteria enter a break in your skin. It can become life-threatening if left untreated, so call your doctor ASAP if you have a red, swollen, tender rash.

Watch for These Symptoms
Cellulitis most often affects the lower leg, but you can get it on other body parts. Common sites include the arm, eye area, breast, and belly. Not everybody has the same symptoms, but these are typical:
- Dull pain or tenderness
- Swelling
- Warmth
- Fever and chills
- Swollen glands and lymph nodes
- Painful rash that may blister and scab
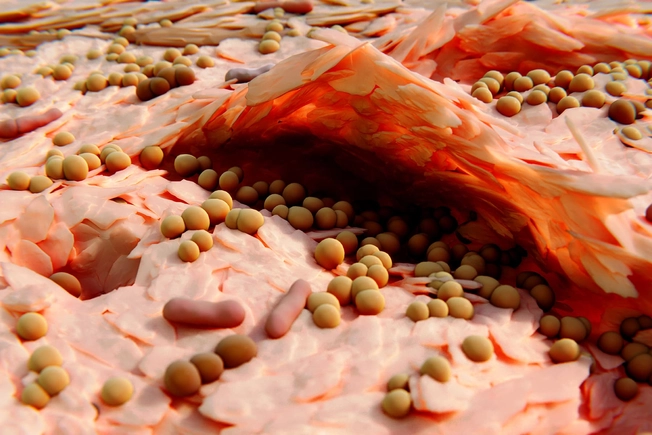
Blame Your Own Bacteria
Streptococcus aureus (strep) and Staphylococcus aureus (staph) are the types of bacteria that usually cause cellulitis. Most of the time, they live on your skin or in your nose and mouth and do no harm. But if you get a cut -- even a tiny one you don’t know you have -- they can enter your body, multiply, and cause infection and swelling.

Diagnosis Is Simple
Your doctor should be able to tell if you have cellulitis just by looking at your skin. Most cases are mild, so tests aren’t needed. But your doctor might order lab tests to get a better idea of what’s going on under your skin. This is usually done for severe cases or people with underlying health problems.

Lab Tests for Cellulitis
Your doctor won’t order lab tests if your case appears mild and treatable. Lab tests are important for those who have:
- Severe skin infection
- Fever or other signs of infection that has spread
- Poor response to the first antibiotic treatment
- Underlying health conditions such as cancer or diabetes
- A recent animal bite

Will You Need an MRI?
Magnetic resonance imaging (MRI) is another test doctors use if you have cellulitis symptoms. It can help them tell the difference between cellulitis and a bone infection called osteomyelitis. You might get one if you have:
- Immune system problems
- Diabetes
- Poor lower-leg circulation
- Lymphedema (chronic swelling)
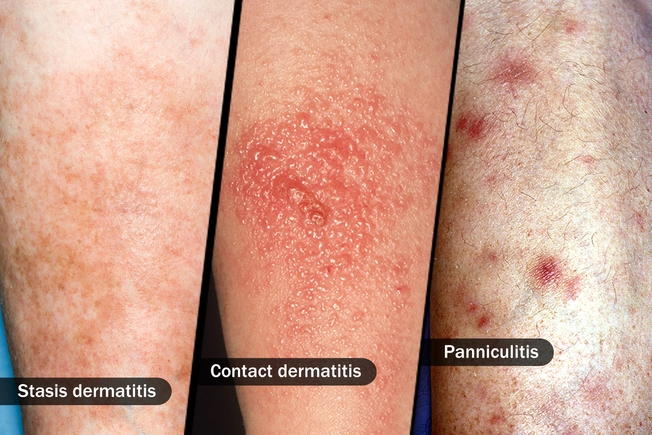
Beware of Misdiagnosis
Be sure your diagnosis comes from an experienced doctor. Cellulitis can look like several other skin diseases and conditions that need different treatments, such as:
- Stasis dermatitis: Swelling related to poor circulation, usually in the lower leg
- Contact dermatitis: Rash caused by something that touched your skin
- Panniculitis: Inflammation of the fat under the skin

Treatment: Antibiotics
Cellulitis requires antibiotic treatment. What you get depends on how serious your conditions is:
Severe: You’ll get antibiotics into a vein in your arm (the doctor will call this intravenous).
Mild: The doctor will give you oral antibiotics, like cephalexin and dicloxacillin.
Once the doctor prescribes an oral antibiotic for you, take it right away -- and finish the medicine as prescribed. Remember, cellulitis can be dangerous without proper treatment.

Treatment: Home Care
Antibiotics are the main form of treatment for this condition, but there are also things you can do at home. If the infection is on your arm or leg, prop that limb up above the level of your heart. That can ease swelling and help it heal faster. You should also keep the infected area clean and dry. It’s OK to shower. Just be sure to pat -- not rub -- the area dry. Also, don’t use antibiotic ointments or creams.

You Should Get Better Soon
If you have a mild case and get quick treatment, you can be out of the woods before long. Expect relief from fever and chills (if you had them) within a day or two after you start your medication. Swelling and warmth may improve within a few days, although these symptoms can last a couple of weeks. Tell your doctor if you don’t feel better within a few days on your antibiotic. You may need different meds and possibly more tests.

Is Cellulitis Contagious?
It isn’t highly contagious. You don’t have to stay away from other people or wipe down all the surfaces you touch. But do wash your hands often with soap and water. And don’t share personal items like towels.

Risk Factors
You’re more likely to get cellulitis if you:
- Have a condition that can cause tiny breaks in your skin, like eczema, athlete's foot, or shingles
- Live with diabetes or a weakened immune system
- Have chronic swelling of your arms or legs (lymphedema)
- Inject drugs
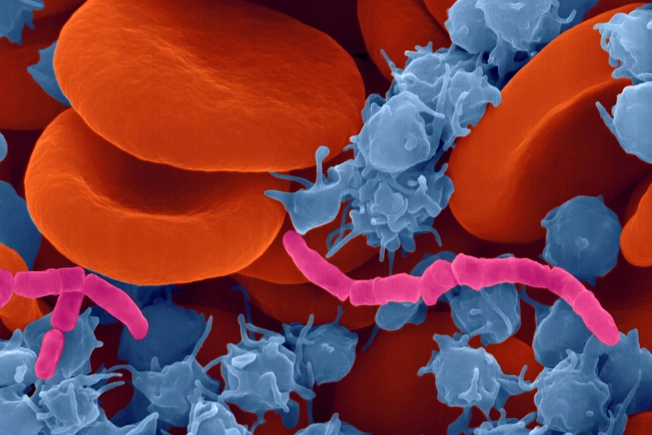
Possible Complications
Early treatment makes it likely that you’ll get completely better without complications. But if you wait too long, a cellulitis infection could become more than skin deep. Bacteria can enter your blood, a condition known as bacteremia. And you can get much sicker from there. So play it safe and call or see a doctor at the first sign of cellulitis.
IMAGES PROVIDED BY:
1) Science Source
2) Science Source
3) Thinkstock Photos
4) Thinkstock Photos
5) Thinkstock Photos
6) Thinkstock Photos
7) Science Source
8) Thinkstock Photos
9) Thinkstock Photos
10) Thinkstock Photos
11) Thinkstock Photos
12) Thinkstock Photos
13) Science Source
SOURCES:
Mayo Clinic: “Cellulitis,” "Cellulite.”
UpToDate: "Skin and soft tissue infection (cellulitis) (Beyond the Basics),” "Cellulitis and skin abscess: Clinical manifestations and diagnosis,” "Panniculitis: Recognition and diagnosis.”
U.S. National Library of Medicine: “Cellulitis.”
Dermatologic Therapy: "Cellulitis: diagnosis and management.”
American Academy of Dermatology: “Stasis dermatitis,” “Contact dermatitis.”
Merck Manual: “Cellulitis.”