Weight Loss Surgery: What to Expect


How Does Weight Loss Surgery Work?
There isn't just one operation. There are several kinds of these metabolic and bariatric surgeries, as doctors call them. They work in the following ways:
- Limit how much food your stomach can hold, so you eat less and lose excess weight.
- Stop your digestive system from absorbing some of the calories and nutrients in the foods you eat.
- Modify and remove parts of the stomach that produce hunger hormones
- All of the above methods.
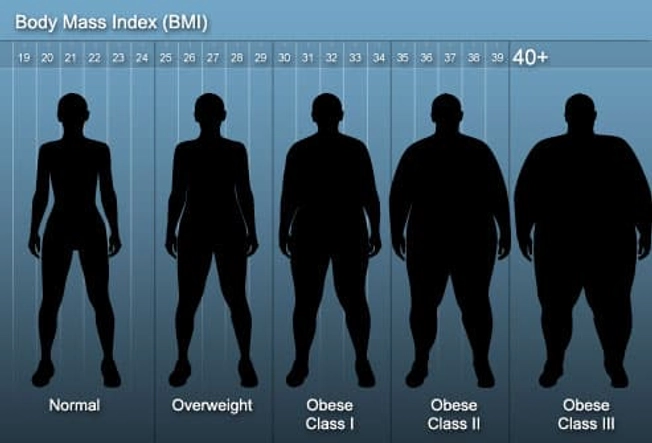
Weight Requirements
You need to meet certain weight criteria to be a candidate for weight loss surgery:
- Body mass index (BMI) of 40 or more (more than 100 pounds overweight).
- BMI of 35-40 or above and have one or more obesity-related conditions such as type 2 diabetes, fatty liver disease, heart disease, high blood pressure, or obstructive sleep apnea. (Your doctor will have the full list.)
- Inability to achieve a healthy weight loss sustained for a period of time with prior weight loss efforts

Types of Weight Loss Surgery
There are different kinds. Some, like the gastric "sleeve" and gastric banding, shrink your stomach's size. They are restrictive surgeries. Other operations, such as the duodenal switch, use the gastric sleeve, along with bypassing part of the intestine, so you absorb less food. Doctors call these restrictive and malabsorptive surgeries.

Weighing the Pros and Cons
Your doctor will screen you carefully to check that you are physically and mentally ready for the surgery, as well as prepared to commit to the big changes needed to keep the pounds off. They will ask about your support system to ensure you're ready for some of the changes you’ll experience after surgery. You'll discuss the risks and benefits of the procedure you're considering. Your doctor may ask you to do some things before the surgery, such as quit smoking, or using alcohol, and make sure your blood sugar is under control.

Preparing for Surgery
Your doctor will tell you exactly what you need to do. You'll typically avoid aspirin or any products that have it, and herbal supplements, 1 week before your operation. You'll need to eat or drink only clear liquids for 24-48 hours beforehand. You'll get general anesthesia during the surgery.
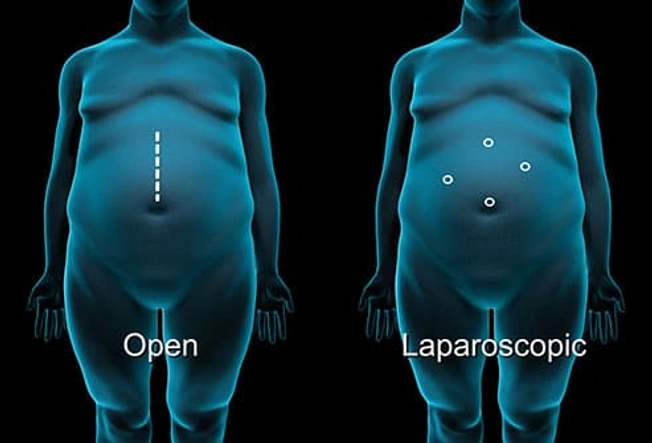
Surgical Methods
Your surgeon will use either the open or the laparoscopic surgical method. These are done with small incisions using laparoscopic and robotic surgery. This helps you recover quickly with less pain and complications. For this procedure, the doctor only needs to make several small, "keyhole" cuts. They’ll use a thin, lighted tool, called a laparoscope, that will show what's going on inside on a monitor in the operating room. For open surgery, you'll get an 8- to 10-inch cut on your belly.
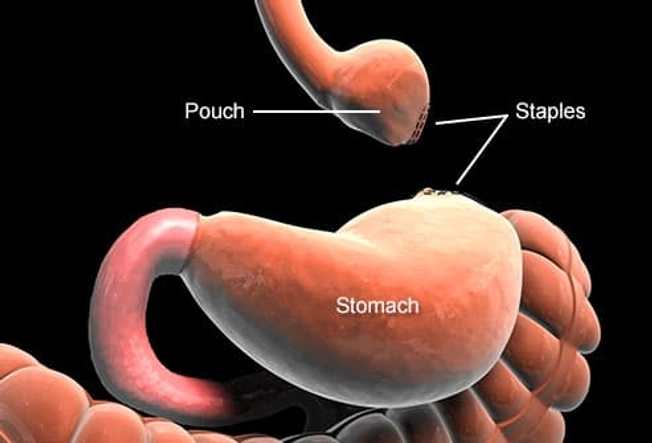
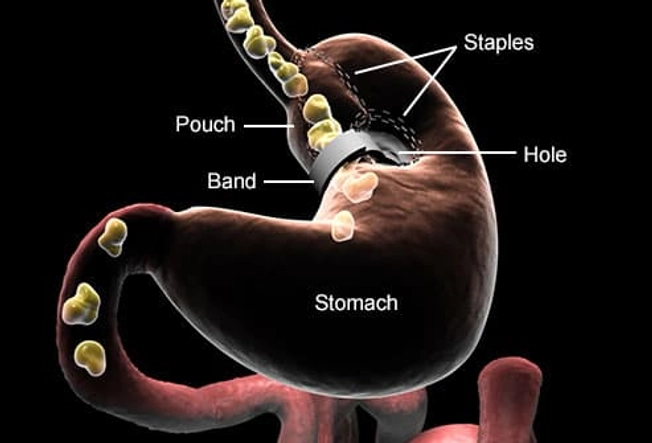
Roux-en-Y Gastric Bypass
During this procedure, your surgeon will use surgical staples to create a small pouch to serve as your new stomach. This pouch will hold about 1 cup of food. The rest of your stomach will still be there, but food won't go to it.
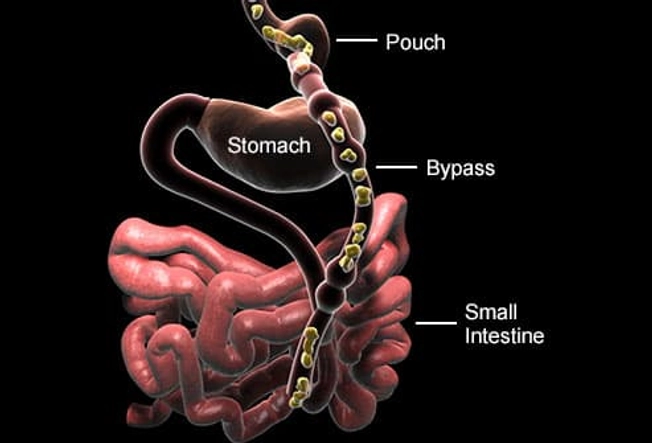
Creating the Stomach Bypass
Next, your surgeon will cut your small intestine beyond the stomach. They will attach one end of it to the small stomach pouch and the other end lower down on the small intestine, making a "Y" shape. That's the bypass part of the procedure. The rest of your stomach is still there. The smaller stomach holds less food so you take in fewer calories, and feel fuller. The intestinal bypass decreases the absorption of food. the stomach delivers chemicals from the pancreas to help digest food that comes from the small pouch. Doctors use the laparoscopic method for most gastric bypasses.
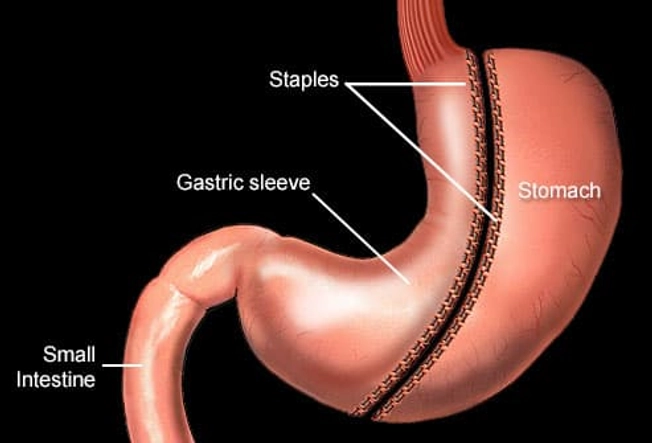
Gastric "Sleeve"
In this operation, your surgeon will take out most of your stomach (80%) and create a tube-shaped stomach, or a gastric sleeve, that is still attached to your small intestine. After the surgery, your stomach will only be able to hold about 2-3 ounces. You'll feel fuller sooner because your stomach is smaller. You also won't be as hungry because part of the stomach that makes the "hunger hormone," called ghrelin, is removed. This is not a reversible procedure.
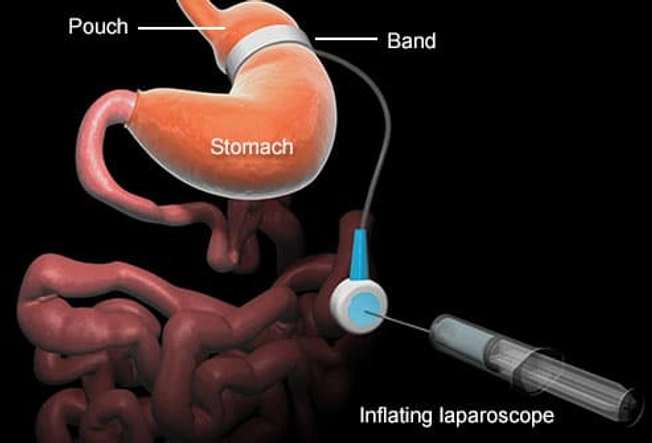
Adjustable Gastric Banding (AGB or Lap-Band)
Your surgeon will wrap an inflatable ring around the top of your stomach. They will inflate the band, squeezing a part of the stomach to create a small pouch with a narrow opening into the rest of the organ. When you eat, food goes through a smaller opening. You can get the band re-adjusted or removed at any time.
Biliopancreatic Diversion
This is a malabsorptive procedure, which means it cuts way down on the calories and nutrients you absorb from food. First, your surgeon will make a small pouch from your stomach. The pouch will only hold about 4-8 ounces, so you'll need to eat a lot less. Then the surgeon will make a bypass that skips the rest of your stomach and most of your small intestine. This procedure bypasses parts of the stomach and intestine that make and are affected by hunger hormones. The effect is decreased hunger and increased fullness. Doctors typically save this operation for people with the most weight to lose, because you miss out on a lot of nutrients.

After the Procedure
You'll stay in the hospital for a short time to make sure you're OK. You'll take pain medications and your doctor will closely watch you for any problems, like low blood sugar, dehydration, or blood clots.

Eating After Weight Loss Surgery
You'll be on a liquid diet at first. After a few weeks, you can eat solid foods. You'll work closely with a nutritionist who's familiar with weight loss surgery to make an eating plan. You’ll need to drink plenty of water and take in more protein than before surgery. You must eat smaller portions and fewer calories. You'll need to make sure you get enough nutrients, which may mean taking vitamins and minerals for life. Your team will tell you what to take and how much.

How Much Weight Will You Lose?
Weight loss may be dramatic in some cases -- as much as a pound a day in the first 3 months. Combination surgery, which causes malabsorption and shrinks the stomach, leads to more weight loss than restriction-only operations.

Other Health Benefits
If you have high blood pressure, diabetes, or other weight-related health problems, they may get better or go away after your surgery. In fact, bariatric surgery is considered a treatment for type 2 diabetes. Work with your doctor to adjust any medications you take for those conditions. Weight loss also can help arthritis, joint pain, or sleep apnea. You may also find it easier to be physically active.

Lifestyle Changes After Surgery
Obesity is a long-term disease and oftentimes relapses. It takes a long-term commitment to make the results last and keep the pounds off. So you must make lifestyle changes you can live with forever. You'll need to eat many small meals throughout the day, and make good nutrition and exercise into daily habits.

Risks of Surgery
All operations carry some risk. For weight loss surgery, there is a small risk for serious complications. People most at risk are those who are older, have a history of deep-vein thrombosis (blood clots), and have a higher BMI's. The best way to avoid complications is to go to all your follow-up visits and stick to your prescribed diet and lifestyle plan.

Complications After Surgery
People who've had weight loss surgery are at risk for problems such as:
- Infection
- Blood clots
- Stomach ulcers
- Gallstones from weight loss
- Not getting enough nutrients
- Problems with the gastric band or sleeve (if you got one of those procedures)
In areas where you lost weight, your skin may sag or be loose. You may want to consider plastic surgery to take up that extra skin, but you might need to wait at least 18 months to do that. Also, some health insurance policies don't cover it.

Dumping Syndrome
After gastric bypass surgery, it is common for food and drinks to move too quickly through your small intestine. Symptoms include nausea, weakness, sweating, faintness, and, sometimes, diarrhea generally within minutes to 1 hour after you eat high-calorie dense foods like simple sugars or fats.

Supplements for Low Nutrient Levels
After malabsorptive weight loss surgery, many people don't absorb vitamins A, D, E, K, B-12, iron, copper, calcium, and other nutrients as well as they used to. Supplements can help you get what your body needs and help prevent conditions like anemia and osteoporosis. Ask your doctor which ones you should take. You will need to have labs done routinely to be sure you are getting enough vitamins and minerals.

Adjusting to Your New Life
You may feel many different emotions after weight loss surgery. You may be happy or excited as you begin to lose weight. You may also feel overwhelmed or frustrated by the changes that you have to make in your diet, activity, and lifestyle. These ups and downs are normal. Talk with your doctor if you have concerns or questions as you get used to your new body.