- Overview
- Types
- Hormonal Methods
- Barrier Methods
- Behavioral Methods
- Medical Methods
- Male Birth Control
- Emergency Contraception
- Side Effects & Complications
- View Full Guide
What Are Your Birth Control Options?


Which Type Is Best for You?
Start with a few questions: How will you protect against STDs? How important are convenience and cost? What about how well it works? Only abstinence is 100% effective, but there are methods that come close if you use them right.

Spermicide
This is a foam, jelly, cream, or film that goes into the vagina before sex that contains a chemical that kills sperm. Some types must be put in place 30 minutes ahead of time. If you use it often, it can irritate the vagina, making infections and STDs more likely. People usually use other types of birth control with it.
Pros: Easy to use, inexpensive.
Cons: May make STDs more likely, and 29% get pregnant during first year of use.

Phexxi
This new nonhormonal birth control gel can be used in place of spermicide. A healthy vagina is acidic, but semen (the fluid that has sperm in it) makes it more alkaline so sperm have a better chance of surviving. Phexxi weakens sperm by helping keep your pH levels low. It comes in 12 prefilled applicators. You can put it in your vagina up to 1 hour before sex.
Pros: It’s easy to use and is about as effective as condoms, and you can use it with condoms for more protection. You can also use it with cervical caps and diaphragms.
Cons: Doesn’t protect against STDs and may irritate some people. You insurance may not cover it. The cost without insurance is about $250-$275 for 12 doses.

Male Condom
The latex condom blocks sperm from entering the woman's body, which protects against pregnancy and some STDs. Of couples who rely on male condoms only, 15% get pregnant in a year.
Pros: Widely available, protects against some STDs, inexpensive.
Cons: Effective only if used correctly every time. Can't be reused.

Female Condom
This is a thin plastic pouch that lines the vagina. A woman can put it in place up to 8 hours before sex. To do that, they would grasp a flexible plastic ring at the closed end and guide it into position. It doesn't work as well as the male condom.
Pros: Widely available, offers some protection against STDs.
Cons: Can be noisy, 21% of users get pregnant, and not reusable. Should not be used with a male condom to avoid breakage.

Diaphragm
This is a rubber dome that women place over their cervix before sex. You should also use a spermicide. Of 100 women who use it, 16 get pregnant in a typical year.
Pros: Inexpensive (a $15-$75 device lasts 2 years).
Cons: Must be fitted by a doctor. No STD protection. Can't be used during your period due to a risk of toxic shock syndrome.

Cervical Cap
This device, also called the FemCap, is similar to a diaphragm but smaller. It slips into place over the cervix. You use it with spermicide. About 15% of women who never had children get pregnant when using the cervical cap. About 30% of women who have had children get pregnant.
Pros: Can stay in place for 48 hours, inexpensive.
Cons: Must be fitted by a doctor. No protection against STDs. You can't use it during your period.

Birth Control Sponge
It's made of foam and contains spermicide. Women can place it against their cervix up to 24 hours before sex. It prevents pregnancy about as well as the cervical cap. But unlike that product or the diaphragm, you don't need to get fitted by a doctor.
Pros: No prescription, effective immediately.
Cons: Can be hard to put in. No STD protection. You can't use it during your period.

Birth Control Pill
The most common type uses estrogen and progestin to prevent ovulation. It's very effective if taken right. About 8% of women who use it get pregnant. You'll need a prescription for it.
Pros: Lighter, more regular periods or no periods, depending on the type. Less cramping.
Cons: Cost ($0-$50 per month). No STD protection. May cause breast tenderness, spotting, blood clots, and raised blood pressure. Some women shouldn't use it due to health risks.

Birth Control Patch
Women who forget to take daily pills may want the Ortha Evra, Twirla or Xulane patch. You wear it on your skin and change it once a week for 3 weeks, then go a week without it. It releases the same hormones in birth control pills and works just as well.
Pros: Lighter, more regular periods with less cramping. No need to remember a daily pill.
Cons: Cost ($0-$50 per month). May cause skin irritation or other side effects similar to birth control pills. No STD protection.
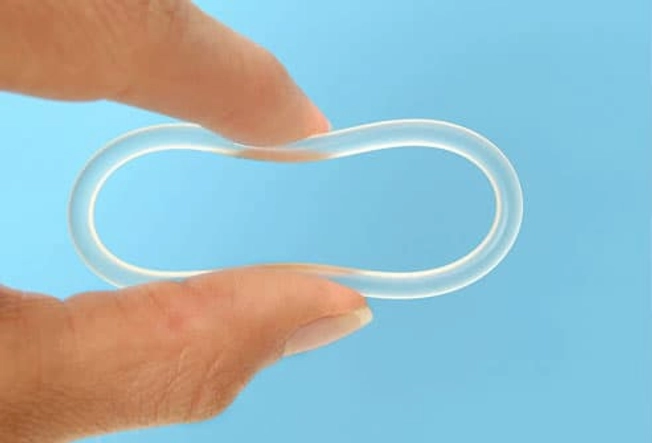
Vaginal Ring
The vaginal ring is a soft plastic ring that goes inside the vagina. It releases the same hormones as the pill and patch, and it works just as well to prevent pregnancy. There are two types available: Annovera and NuvaRing. Annovera can be reused after a 1-week break each month. NuvaRing is replaced each month.
Pros: Lighter, more regular periods. Less-frequent replacement.
Cons: Cost ($30-$50 per month). May cause vaginal irritation or other side effects similar to pills and the patch. Doesn't protect against STDs.

Birth Control Shot
It's called Depo-Provera, and it's a hormonal shot that protects against pregnancy for 3 months. For the typical couple, it works better than the birth control pill. Only 3% of users get pregnant in a year.
Pros: Injected only 4 times per year, highly effective.
Cons: Cost (about $240 per year). May cause spotting and other side effects. Doesn't protect against STDs.

Birth Control Implant
Nexplanon is a matchstick-sized rod that a doctor places under the skin of a woman's upper arm. It releases the same hormone that's in the birth control shot. The failure rate is less than 1%.
Pros: Protects against pregnancy for 3 years and then must be removed. Highly effective.
Cons: More expensive up front ($400-$800 for exam, implant, and insertion). May cause side effects, including irregular bleeding. Doesn't protect against STDs.
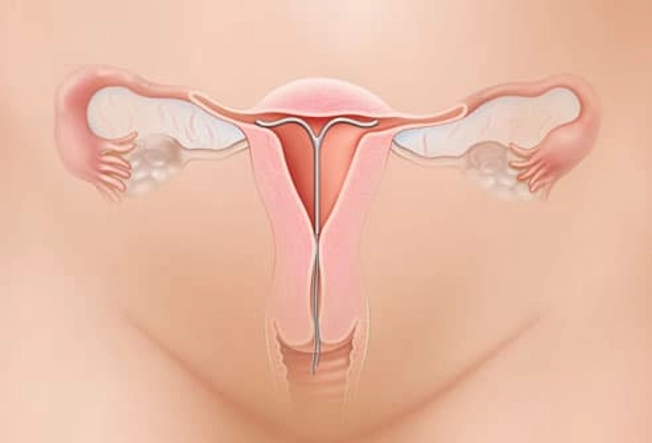
IUD
That stands for intrauterine device. It's placed inside a woman's uterus. The nonhormonal copper IUD, ParaGard, works for as long as 10 years. The hormonal IUDs must be replaced after 3-5 years. Both types make it harder for sperm to fertilize the egg. Fewer than 8 in 1,000 women get pregnant.
Pros: Long-lasting, low-maintenance. Hormonal IUDs can make periods shorter and lighter.
Cons: Irregular or heavier periods. Copper IUDs can make periods more painful. More expensive up front, may slip out, may cause side effects.
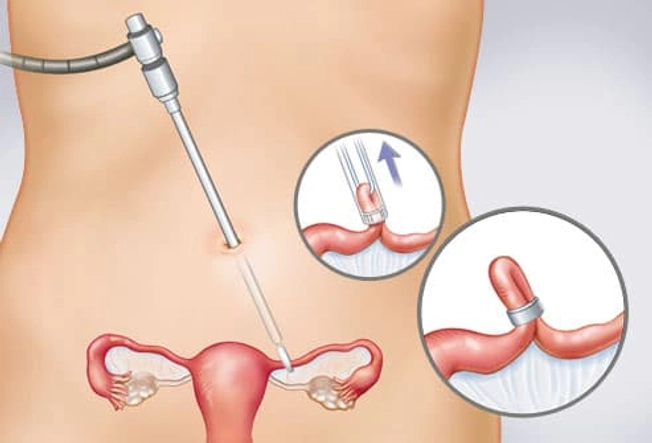
Tubal Ligation
If you're sure you won't want to get pregnant, you may be ready for permanent birth control. The operation for women is called tubal ligation, or "having your tubes tied." A surgeon closes off the fallopian tubes. This prevents an egg from meeting sperm. (The banding method is shown here.)
Pros: Permanent, nearly 100% effective.
Cons: Requires surgery, may not be reversible, expensive. Doesn't protect against STDs.
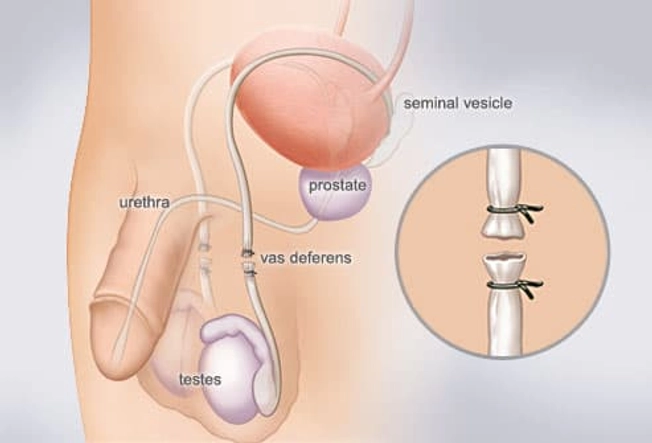
Vasectomy
Other than condoms, a vasectomy is the only birth control option for men. A doctor surgically closes the vas deferens, the tube that carries sperm from a testicle. This prevents the release of sperm but doesn't affect ejaculation.
Pros: Permanent, cheaper than tubal ligation, almost 100% effective.
Cons: Requires surgery, not effective immediately, may not be reversible. Doesn't prevent STDs.
Emergency Contraception
This method works within a few days after sex to help avoid pregnancy. This is an option if you didn't use contraception or if a woman suspects their usual method failed. There are lots of types to choose from, including brand-name pills or generic versions. You can get some of them over the counter or by prescription. You may also get a copper IUD inserted by a medical professional..

Options for Older Women
If you're over age 35 and smoke or are obese, the combination birth control pill, the patch, and the ring are not recommended. Ask your doctor about safe alternatives. If you're nearing menopause, the birth control shot has an added benefit: It may relieve some of the symptoms of perimenopause.

Withdrawal
"Pulling out" is the age-old method that relies on the man withdrawing their penis from the vagina before ejaculation. If it's done correctly every time, about 4% of users get pregnant in a year. But with more typical use, about 18% get pregnant.
Pros: Free, no need for devices or hormones.
Cons: May be hard to do correctly. No protection against STDs.

Ovulation Predictor Kits
A lot of women who want to get pregnant use these to figure out when they're most fertile. The kit comes with a urine test that checks how much luteinizing hormone (LH) you have. LH surges 24 to 38 hours before you ovulate, which is when you're most likely to get pregnant. To try to prevent pregnancy, don't have sex when you're ovulating.
Pros: No drugs, inexpensive.
Cons: Limits spontaneous sex, and the odds of getting pregnant are high.
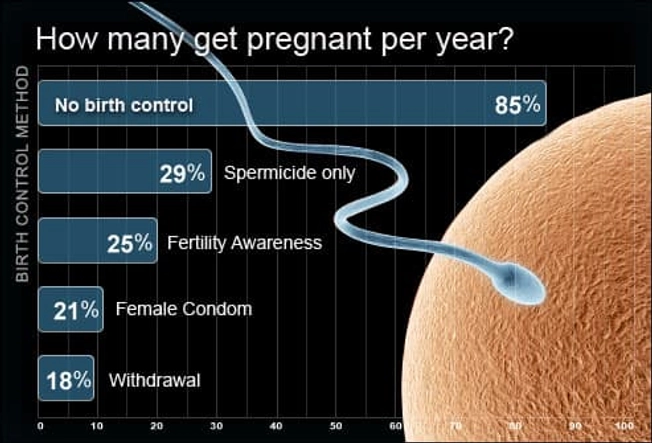
Least Effective Methods
Without using any form of birth control, 85% of sexually active couples will get pregnant within a year. Even the least effective birth control options greatly lower that number.
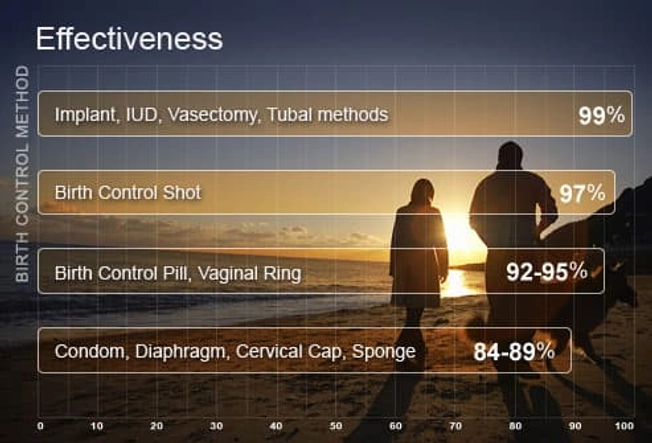
Most Effective Methods
If you don't want to get pregnant, it really matters how correctly you use your method of birth control. The most effective types are those that you don't have to think about.