The female breast is an organ that changes with puberty, with the monthly menstrual cycle, and with pregnancy. It also continues to change with age.
Most changes in your breasts are perfectly normal and no cause for concern. But some changes need medical attention. Chief among these are breast pain and lumps.
Breast Lumps
Breast lumps come in many forms, including cysts, adenomas, and papillomas. They differ in size, shape, and location, as well as in causes and treatment. About half of all women have lumpy breasts, or fibrocystic change. They are more common during the premenstrual period and usually disappear after menopause. Most lumps are benign and do not signal cancer; however, any time you find a new or unusual lump, have your doctor check it to make sure it is not precancerous or cancerous.
Researchers are studying the incidence of breast lumps in women using hormone replacement therapy (HRT). In combination HRT, women take the hormones estrogen and progestin to ease the symptoms of menopause. In 2002, a study called the Women’s Health Initiative discovered that HRT often resulted in more harm than good. Taking both hormones was shown to increase the risk of breast cancer and change the breast's structure, increasing breast density and making mammograms harder to read. This could make finding cancer more difficult. To put this into numbers, if 10,000 women took combined HRT for a year, this would add up to about 8 more cases of breast cancer per year than if they had not taken hormone therapy (HT).
Cysts, which can be large or small, are often harmless, fluid-filled sacs that may be painful.
After menopause, many cysts shrink or disappear. You should immediately have your doctor check any lumps that form after menopause.
Fibroadenomas are the most common benign breast tumors in women under 25 and occasionally in adolescents. These tumors are usually round, several centimeters across, and mobile. They tend to regress after menopause. Your doctor may recommend removal if the lump persists, gets larger, or if you are anxious about it. Tests will be done to check for cancer when it is removed.
Nipple adenomas are tumors of the nipple area. They vary in appearance, sometimes come back after being removed, and are sometimes associated with cancer. An intraductal papilloma is an uncommon small growth in the lining of the milk ducts near the nipple. Usually seen in women over 40, papillomas produce a discharge, which may be bloody.
Breast Self-Exams and Mammograms
The ACS states that research has not shown a clear benefit of performing regular breast self-exams. If you decide to perform breast self-exams, your doctor should go over how to perform them with you. Premenstrual changes can cause temporary thickening in breast tissue that disappears after your period, so your doctor may tell you to wait until a few days after your period to do them.
A breast self-exam is easiest in the shower, using soap to smooth your skin. Look for dimpling. Using light pressure, check for lumps near the surface. Use firm pressure to explore deeper tissues. Squeeze each nipple gently; if there is any discharge -- especially if it is bloody -- consult your doctor.
Any time you find a new or unusual lump in your breast, have your doctor check it to make sure it is not cancer. Most lumps are harmless. The best test for distinguishing a cyst from a solid tumor is ultrasound; a needle biopsy may also be done.
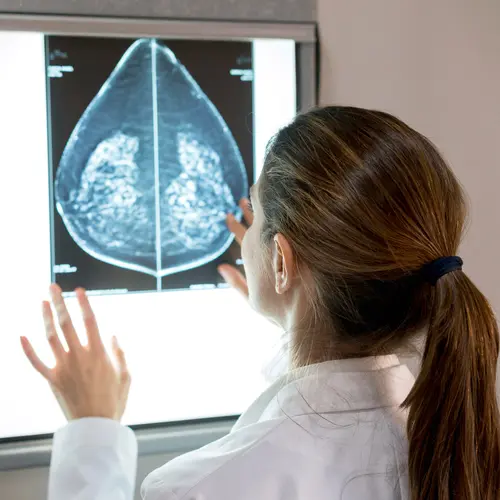
Mammograms -- detailed X-ray pictures of the breasts -- can reveal tumors too tiny to be felt by hand. There is disagreement as to when a woman should start getting mammograms: Some doctors say age 40; others say not until age 50. The American Cancer Society recommends women ages 40 to 44 should have a choice to start yearly screening mammograms if they would like. Women ages 45 to 54 should have a mammogram each year. and those 55 years and over should continue getting mammograms every 1 to 2 years.. The USPSTF recommends routine screening for women starting at 50. If you have a family history of breast cancer, especially in your mother or sister, your doctor may want you to start them earlier. Three-dimensional mammograms, to be used along with traditional digital mammograms, are also available in some screening centers.
Breast Pain
Breast pain can have many causes, including the normal swelling of breast tissue during the menstrual cycle. Other causes include infection or injury; growths, including cancer; and perhaps diet.
The general swelling of breast tissue with your period can be painful, but it is not dangerous, and no treatment is necessary if you can tolerate the discomfort. Each monthly cycle brings about changes in hormones, including more estrogen and progesterone, that bring more fluid into the breasts, expanding tissue, stretching nerve fibers, and causing pain. Some women have this painful swelling just before their periods, with symptoms easing near the end of the menstrual flow. Others have it as a side effect of birth control pills.
Trauma and infection in the breast have the same symptoms you would see elsewhere in your body. Infections tend to become walled off from surrounding tissue, producing small abscesses. This may give them the appearance of cysts. If you think you have an infection, see your doctor. Your doctor will usually prescribe antibiotics, although many times the infection will come back and may require the removal of the infected tissue.
Cysts may produce pain, but breast cancer rarely does -- although pain does not rule out the possibility of cancer.