- Overview & Types
- Symptoms & Diagnosis
- Treatment
- Living With
- Related Conditions
- Type 2 Diabetes
- Type 1 Diabetes
- Gestational Diabetes
- Appointment Prep
- View Full Guide
Diabetes and Eye Problems

How Diabetes Affects Your Eyes
The main problem is high blood sugar (glucose). Diabetes means your body doesn’t make or use insulin correctly, which raises blood sugar. When this first happens, it can change the level of fluid in parts of the eye that help you focus. You might have no symptoms, or your vision might be blurry for a few days or weeks. It usually returns to normal once your treatment plan brings your glucose levels back down.

Long-Term Effects of High Glucose
Over time, high blood sugar levels can damage the very small blood vessels at the back of your eyes. The vessels leak fluid and cause swelling, pressure, and other problems. If your glucose levels are high enough, the damage can start before signs of diabetes show up in other parts of your body. This can lead to four diabetes-related eye problems: retinopathy, macular edema, glaucoma, and cataracts.

Early Diabetic Retinopathy
In early nonproliferative diabetic neuropathy, or NPDR, blood vessels bulge and leak into the inner lining of the back of the eye (known as the retina). Your nerve endings might swell, too. You may not have symptoms at first. Talk to your doctor about eye health if you have diabetes or you know your blood sugar is high. It’s important to start managing it early.
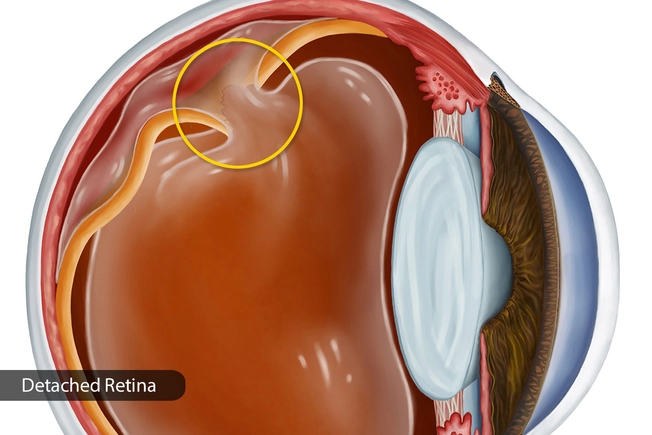
Advanced Diabetic Retinopathy
Here, the blood vessels at the back of your eye start to close. New ones grow in the retina, but they’re damaged. They can leak into the vitreous, the jelly-like substance in the middle of your eye. You might see dark spots or streaks that seem to float through your line of vision. If you don’t get treatment right away, scar tissue may form. This could separate the retina from the back of your eye, which is serious.
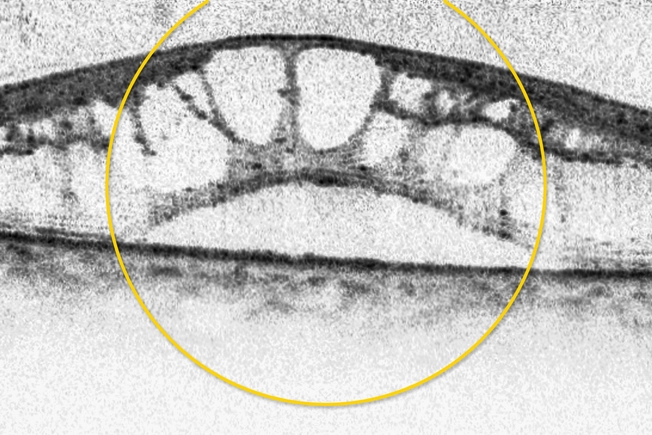
Diabetic Macular Edema
Retinopathy sometimes leads to fluid in an important part of the retina called the macula. You need it to drive a car, recognize faces, and read. When your macula swells, your vision could blur and you may lose some or all of your sight. About half of people who get diabetic retinopathy will also get DME.
Glaucoma
There are several types, but they all put pressure on the optic nerve at the back of your eye that connects to your brain. You may not have symptoms at first, or you might start to lose your side vision. But you don’t notice because it happens so slowly. If you don't treat it, the pressure can lead to permanent vision loss.
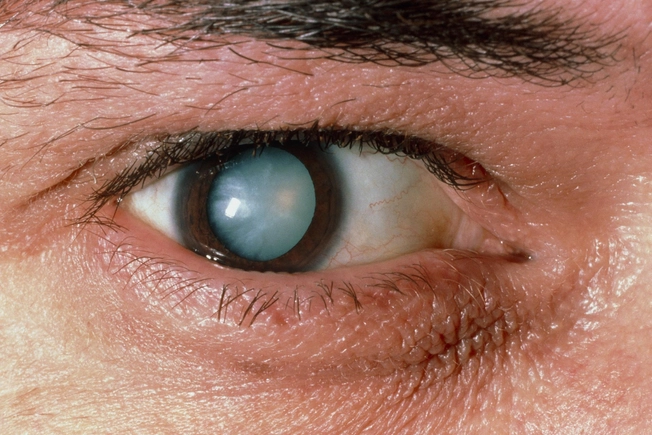
Cataracts
When the lens of your eye looks cloudy, it’s called a cataract. This blocks light, and everything looks hazy. Poor control of blood sugar can speed up the process. You're more likely to get cataracts with diabetes -- and you'll probably get them at a younger age. Surgery can replace the cloudy lens with a clear artificial one, but diabetic retinopathy sometimes gets worse afterward if your blood sugar isn't under good control.

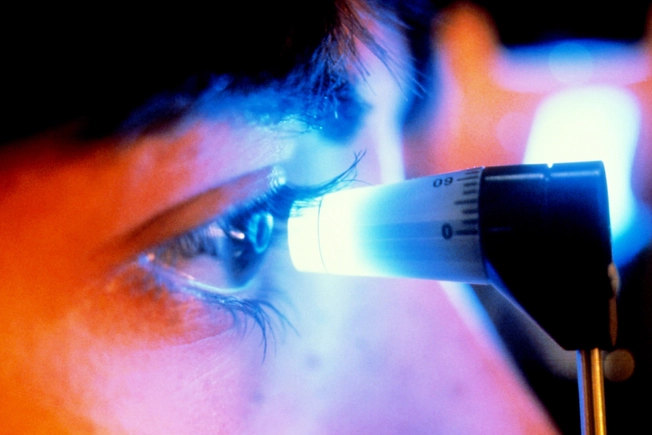
Diagnosis of Diabetic Eye Disease
If your doctor thinks you have diabetic eye problems, they’ll test your vision and measure the pressure in your eyes. Medicated eye drops will widen your pupils -- the part of your eye that lets light in -- so they can look at the back of your eye. The doctor might inject a dye into your arm. The dye can show any leakage in the small blood vessels of your eye. Your vision might be blurry for a few hours after the exam.

Early Treatment
Your doctor might suggest more frequent eye checkups to make sure your condition doesn’t get worse. The only treatment at this point might be diabetes management. Typically, you’ll keep track of and try to control your blood sugar, cholesterol, and blood pressure. Prescription medication, exercise, eating better, and quitting smoking can help.

Laser Treatment
Panretinal photocoagulation uses a laser to destroy areas of your retina where abnormal blood vessels have grown. Focal treatment, which is less common, uses a laser to seal blood vessels and stop them from leaking and growing. These surgeries can keep vision loss from getting worse.
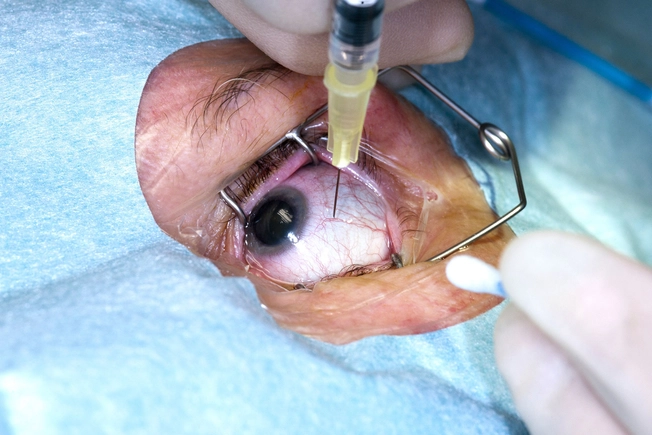
Anti-VEGF Drugs
The doctor injects shots of medicine into the jelly inside your eye. This keeps your eye from growing new blood vessels. Though you tend to need fewer shots over time, it isn't a cure. You typically need regular shots to maintain results.

Vitrectomy
In the late stages of diabetic retinopathy -- if your retina has detached or a lot of blood has leaked into your eye -- your doctor may suggest this operation to remove scar tissue, blood, and cloudy fluid inside your eye. Vitrectomy can improve your vision.

Who Gets Diabetic Eye Disease?
The longer you have the disease, the more likely your chances are. Your odds are higher if you don't have good control of your blood sugar or you have high blood pressure or cholesterol. Your risk is also greater if you smoke.

Don't Wait for Symptoms
When your blood sugar is high or when you start using insulin, you may have blurry vision. There may be damage caused by diabetes even if your vision seems normal. That's why you should get an eye exam at least once a year.

See Your Doctor
Get to an ER right away if you suddenly lose sight (including a "curtain" coming down over your vision), see flashing lights, double vision, or severe eye pain or pressure, you hould see a retinal specialist immediately but not necessarily go to the emergency room. Make an appointment with your eye doctor as soon as you can if you have these:
- Blurry or hazy vision
- Spots, floaters, or shadows
- Waviness or distortion of straight lines
IMAGES PROVIDED BY:
1) Getty
2) PRinc
3) PRinc
4) PRinc
5) Medical Images
6) PRinc
7) PRinc
8) Getty
9) Getty
10) Science Source
11) Science Source
12) Getty
13) Getty
14) Getty
15) Getty
SOURCES:
CDC: “Common Eye Disorders.”
National Diabetes Information Clearinghouse: "Prevent diabetes problems: Keep your eyes healthy."
FamilyDoctor: "Diabetes: Eye Care."
Mayo Clinic: “Diabetic Retinopathy.”
MedlinePlus: "Diabetes - eye care."
National Eye Institute: “Injections to Treat Diabetic Retinopathy and Diabetic Macular Edema,” “Diabetic Retinopathy,’ "Diabetic Eye Disease FAQ," "Facts About Diabetic Retinopathy."
National Institute of Diabetes and Digestive and Kidney Diseases: “4 Steps to Manage Your Diabetes for Life,” “Diabetic Eye Disease.”
Preventblindness.org: “Diabetes and Your Eyes,” “Diabetes-related Retinopathy.”
American Diabetes Association: "Eye Complications," "Eye Care."
Diabetes Care: "Position Statement: Diabetic Retinopathy (2003)," "Ocular Anti-VEGF Therapy for Diabetic Retinopathy: Overview of Clinical Efficacy and Evolving Applications," "Ocular Anti-VEGF Therapy for Diabetic Retinopathy: The Role of VEGF in the Pathogenesis of Diabetic Retinopathy."
RNIB: "Anti-VEGF treatment."
U.S. News & World Report: "Diabetes Seems to Heighten Glaucoma Risk."