- Overview & Types
- Symptoms & Diagnosis
- Treatment
- Living With
- Related Conditions
- Type 2 Diabetes
- Type 1 Diabetes
- Gestational Diabetes
- Appointment Prep
- View Full Guide
Meal Planning Tips to Control Blood Sugar Levels


Make a Plan
Having diabetes makes it important to keep a careful eye on your blood sugar (glucose) levels and your weight. It can be tough. But knowing what to eat, when to eat, and how much to eat can make it easier. The key is to find what works best for your tastes, your lifestyle, and your budget.

Find the Right Balance
With diabetes, your diet should be high in nutrients and low in fat and calories. There are many ways to do that, like going low-carb, low-fat, or vegetarian. Shoot for a 50-25-25 split, with the largest section filled with non-starchy vegetables (like peppers or spinach), and a section of protein, and one of grains and starches (like beans or potatoes). A daily serving of fruit or dairy and small amounts of healthy fats are OK, too.

Time Your Meals
When you eat is important, especially if you use mealtime insulin. Aim to eat at the same times every day. Try to keep the amount of food about the same, too. Having one big meal at the end of the day or spacing your meals unevenly can affect your blood sugar and your medication. Your doctor or dietitian can help you set the right times to eat.

Don’t Skip Meals
If you take medicine for diabetes, going too long without eating can lead to seriously low blood sugar levels. And running out the door in the morning without breakfast can set the wrong tone for the day and make you want high-calorie foods later. That can make managing your glucose levels -- and your weight -- harder.

Watch Your Portions
A key part of any diet plan is proper serving sizes. When you first start to pay attention to the amount, your eyes may not be accurate enough -- especially when you’re hungry.
For example, a serving of meat like chicken is only about the size of the palm of your hand. It’s best to use a few tools -- like measuring cups, scales, or spoons -- until you get the hang of it.

Consider How Active You Are
Exercise burns glucose and helps your body use insulin. That means it can help control your blood sugar. But it also can affect how much you should eat and how much medicine you need. Talk with your doctor about what your levels should be when you exercise and how often to check them. Your doctor can also help you figure out how to time your meds and meals around your workouts.

Check Your Levels Regularly
If you take insulin, it’s best if it starts to work about the same time glucose from your food hits your bloodstream. So the ideal time to take it is about 30 minutes before you eat. But many things can affect your blood sugar, like exercise, being sick, or stress. It’s important to keep a close eye on your levels and make sure you’re getting the right amount of insulin.

Count Carbs
Foods with carbs affect your blood glucose more than anything else you eat. One way to manage this is to figure out how many grams of carbs are in a meal and base your dose of insulin on that amount. To start, keep track of your meals and check your blood sugar before you eat. Then check it again in about 2 hours to see how different foods affect you. This can help you and your medical team figure out the right amount of carbs for you.
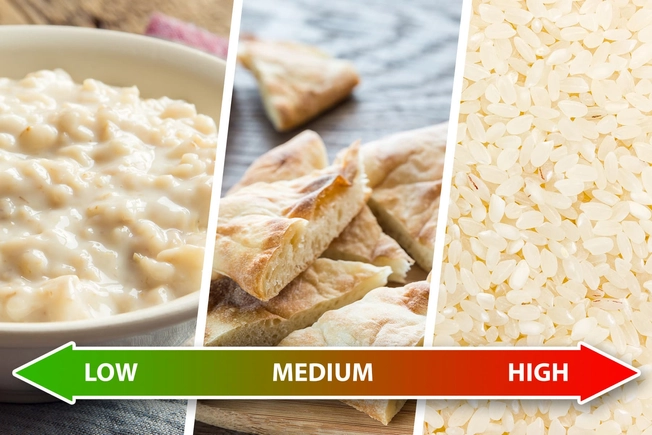
Use the Glycemic Index (GI)
This lets you predict how a food will affect blood sugar. The lower a food’s GI level, the better, and you can balance out high-GI foods with low- and medium-GI ones. Low-GI foods include oatmeal, pasta, sweet potatoes, corn, carrots, peas, most fruits, and non-starchy vegetables.
Medium-GI foods include whole-wheat or rye bread, pita, and brown, wild, or basmati rice.
High-GI foods include white bread, white rice, russet potatoes, pretzels, popcorn, melons, and pineapple.

Get Plenty of Fiber
Foods that are high in fiber take longer for your body to digest, so they affect your blood sugar levels more slowly. They’re also part of a healthy, balanced diet. Good choices include non-starchy vegetables (think spinach, collards, or kale), fruits (especially citrus, like grapefruits or oranges), beans, and whole grains.

Limit Unhealthy Beverages
Sweetened drinks, like soda or sports drinks, can spike your blood sugar. And they give you lots of empty calories. On the flip side, alcohol can make your levels too low because it affects how your liver releases sugar into your bloodstream. If your blood sugar is under control and your doctor says it’s OK, an adult beverage is fine from time to time. Just make sure to eat beforehand and watch your levels closely, especially before bed.

Plan for When You’re Sick
Your body’s natural way of fighting off illness can raise your blood sugar, so you might need to make some changes to your treatment when you're under the weather. Your doctor can help you prepare for it and manage it. For example, you might need to check your blood sugar more often, or sip juice or a sports drink to keep your blood sugar where it needs to be.

Use the 15-15 Rule
If you have a sudden drop in blood sugar, this rule can get you back on track without sending your levels too high.
The idea is to eat or drink something with at least 15 milligrams of carbohydrates, wait 15 minutes, then check your blood sugar to see if it's back up to at least 70 milligrams per deciliter (mg/dL). A tablespoon of sugar or honey or 4 ounces of juice or soda might do.
But don’t eat until you’re full. That can send your levels too far in the other direction.
If You Need Help
It can be hard to find a way to control blood sugar. Medical nutrition therapy, from a registered dietitian nutritionist, may help. The nutritionist will talk with you about your eating habits and lifestyle, then help you come up with a personalized plan. You’ll have follow-ups to talk about your progress and adjust your plan.
Medicare covers this type of therapy for people with diabetes. Private insurers might cover it too. Ask yours.