The most common treatments for wet age-related macular degeneration (wet AMD) are designed to counter the proteins which contribute to the development of AMD. Your doctor gives you this therapy through an injection directly into your eye.
How often you need these injections depends on your case of wet AMD. It could be as often as every few weeks or as far apart as every few months. Here’s what to know about this treatment.
What’s in the Injection
Anti-angiogenic drugs. If you have the wet form of AMD, your doctor will inject these medications into your eye. They stop new blood vessels from forming and stop the leaking from the abnormal vessels that cause wet AMD.
Vascular endothelial growth factor (VEGF) is the main protein that causes new blood vessels to form in the macula in wet AMD. VEGF inhibitors reduce leakage from blood vessels, prevent their growth, decrease swelling of the retina, reduce vision loss, and improve vision in wet AMD.
The treatments include:
- Aflibercept (Eylea)
- Bevacizumab (Avastin)
- Pegaptanib (Macugen)
- Ranibizumab (Lucentis)
Inhibition of angiopoietin-2 (Ang-2), another protein involved in blood vessel formation, helps stabilize these fragile new blood vessels so they don’t leak. It also makes vessels less sensitive to the effects of VEGF.
VEGF/Ang-2 inhibitors include:
- Faricimab-svoa (Vabysmo)
Some people who get these drugs have been able to regain vision that they lost from AMD. You may need to repeat the treatment on follow-up visits.
All of these medications stop blood vessel growth, though they do it in slightly different ways. They’re similarly effective and come with similar risks. Your doctor will help you decide which is best for you.
The main side effect risks are infection or inflammation in the eye, bleeding into a gel inside your eye called the vitreous gel, and retinal detachment.
Before the Injection
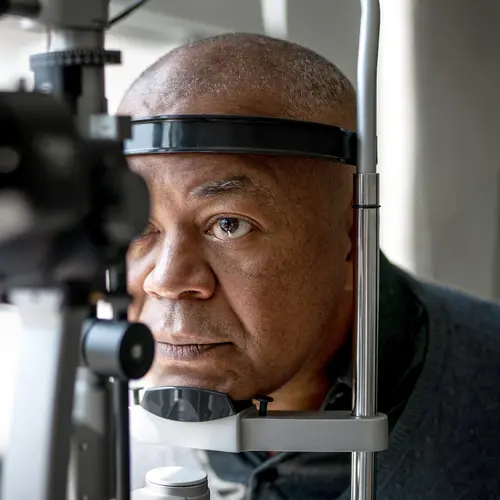
Your eye doctor will confirm you have wet AMD with a dilated eye exam and imaging before you begin treatments. When it’s time for your first treatment, you can get the injection in your doctor’s office during an appointment that usually lasts less than an hour. The procedure itself will take about 15 minutes.
First, your doctor will numb your eye using eye drops. Then they’ll clean your eye with a yellow iodine solution. To keep you from blinking during the injection, your doctor will put a small device on your eye to hold your top and bottom eyelids out of the way.
Getting the Shot
The needle your doctor uses to give you the injection is very small and thin. The injection happens very quickly, in less than a second.
Your doctor will ask you to look up and then will put the needle into the white part of your eye (the sclera). They’ll insert the needle as far as the vitreous part of your eyeball -- a jelly-like substance in the middle of your eye -- to inject the treatments like those that target VEGF or Ang-2.
Usually, the injection is painless. Some people feel a little discomfort or pressure. As the treatment mixes with the fluid in the middle of your eye, you might see wavy lines.
Once the needle is out, your doctor will put a sterile cotton tip over the injection site for about 10 seconds to put pressure on it and keep fluid from escaping. Then they’ll flush your eye with a solution to lubricate it and keep it from getting irritated.
Follow-Up Care
You may see an improvement in your wet AMD symptoms within a week of your injection. You may be sore for a few days following your injection. Your vision may be slightly foggy. You can take over-the-counter pain relievers such as acetaminophen or ibuprofen to help with the discomfort. Putting a cool washcloth on your eyes for about 10 minutes every half hour may also help soothe soreness.
If the needle hit a blood vessel in your eye as your doctor injected it, you may have some redness in the whites of your eye for up to 2 weeks. As long as you don’t have pain or vision problems, this is a harmless side effect.
If you have certain side effects after your injection, tell your doctor so you can come in for a check of your eyes. Some symptoms to watch for are:
- Eye pain
- Sensitivity to light
- Vision changes
- More eye pressure
- “Floaters” in your vision
Pain, sensitivity to light, and vision changes could be signs of an infection. These complications are rare, but if you have them or any of the symptoms listed above, you should tell your eye doctor