The macula is in the center of your eye’s retina. It lets you see what’s right in front of you in sharp focus.
But if you have macular edema, fluid collects in the retina and causes the macula to swell. Your central vision may become blurry. Reading a book, watching TV, recognizing faces, or telling the difference between colors can be hard.
There are two types of common macular edema: diabetic and cystoid. Early treatment can help you see better and even save your sight.
What’s the Difference Between Diabetic and Cystoid Macular Edema?
They both have “macular edema” in the name because they both involve swelling in that part of the retina. But that’s largely where the similarities end, says Talia Kaden, MD, an ophthalmologist at the Manhattan Eye, Ear and Throat Hospital in New York.
The causes, treatments, and the outcomes can be very different.
Think of it like chest pain, Kaden explains. That can be caused by something like a heartburn or a heart attack. They both have sharp pain in common, but they happen because of very different reasons. And your outcome can be very different, too.
Both types of macular edema can be serious. But diabetic macular edema (DME) is a more significant disease and involves a lot more treatment and management, Kaden says.
What Causes Diabetic Macular Edema?
Type 1 and type 2 diabetes cause DME. Constant high blood sugar weakens connections between cells in small blood vessels called capillaries. They begin to leak fluid into the macula.
If you’ve had diabetes for a long time or it's not controlled well, the higher your chance of getting DME. Your risk is raised if you have these other health problems, too:
- High blood pressure
- High cholesterol
- Poor kidney function
People often are surprised to hear they have serious DME because they don’t notice symptoms or they’re very mild, Kaden says.
But what you don’t know can hurt you. Diabetic eye disease is the leading cause of vision loss in working-age adults. That’s why it’s so important to get yearly dilated eye exams, preferably by a retina specialist, she stresses.
Catching problems early is key to successful treatment.
What Causes Cystoid Macular Edema?
The most common culprit for cystoid macular edema (CME) is cataract surgery. Up to 20% of people who have the operation get it. Usually, it happens within 6-10 weeks afterward. It’s more likely if you have a complicated surgery, Kaden says.
But other things cause CME. These include:
- Eye surgery for glaucoma or retina surgery
- Medications like niacin and certain chemotherapy drugs
- Uveitis, an immune system problem that causes eye inflammation
- Retinitis pigmentosa, a genetic eye disease
- Age-related macular degeneration (AMD). This can happen when you have what’s called “wet” AMD, when fluid leaks into or under the retina.
How Are They Diagnosed?
Your retina sits at the back of your eye and changes light into signals that go to your brain. It’s like a layer cake, and fluid can collect anywhere between the layers or even under the retina, Kaden says.
In CME, fluid collects in a specific layer. It may look like cysts to your doctor.
Both are diagnosed in similar ways. These include:
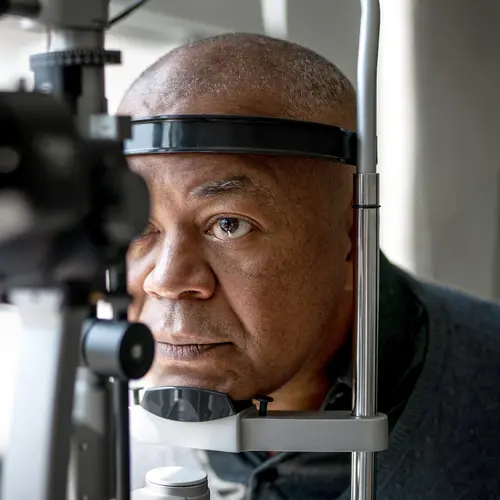
- Dilated eye exam. Your doctor gives you eye drops to widen your pupils to see more of your retina.
- Optical coherence tomography (OCT). This test uses a machine to take pictures of the layers at the back of your eye. It can be used to diagnose macular edema and monitor it.
- Fluorescein angiogram. This test lets your doctor see blood flow in your retina. Your doctor will inject a dye into your arm. It travels through your bloodstream to your eyes. Your doctor takes pictures as the blood flows through your retina.
What’s the Treatment?
If the CME is caused by medication, your doctor may change the drugs you take.
If the cause is cataract surgery, it’s treated with steroid or nonsteroidal eye drops.
A retina specialist may treat the CME with injection medication if eye drops don’t help.
Eye drops won’t work for DME, Kaden says. The first thing you should do is get your diabetes and any other related health problems under control.
You’ll need to find a retina specialist to treat your DME.
Here are some questions to ask:
What is the most common treatment for DME?
Anti-vascular endothelial growth factor (Anti-VEGF) drugs. VEGF is a protein your body makes. Too much of it can contribute to abnormal growth of blood vessels in your eyes. Controlling it can help protect your vision or even improve it.
How do you get it?
It’s an injection you get in the white of your eye.
That may sound scary, but Kaden explains that your eye will be numbed with drops and the needle is very small.
Kaden says her patients say the worst part is a solution that cleans the eye to prevent infection. Most people describe it as feeling like they have soap in their eyes. She tells her patients it feels like that because you actually do have soap in your eyes. Your doctor will do their best to flush it out before you leave the office, Kaden says.
Do I need just one shot?
People usually need a shot once every 4-6 weeks for the foreseeable future.
Your doctor will work out a plan based on your needs.
What Can You Expect?
Most of the time, CME goes away in a few weeks and doesn’t come back.
DME usually responds well to the injections. But it really depends on how much swelling you have to start with and how well you control your diabetes. Treating it in time and sticking with it helps, too.
Kaden says she sees people with CME for a couple of months and that’s it. But she sees her DME patients for life.