Leg pain and other symptoms of periphery arterial disease (PAD), which happens when narrowed blood vessels reduce the flow of blood to your limbs, can make it hard to get enough sleep. So can certain sleep disorders that are linked to PAD.
PAD is most often caused by atherosclerosis, which is when fats and other debris from your bloodstream build up inside your arteries. It usually affects the blood supply to your legs, but sometimes it involves your arms.
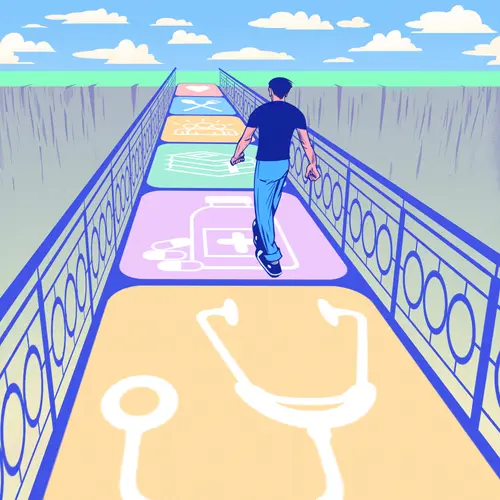
Treatment for PAD, and for any related conditions you may have, can help you get the rest you need.
What Are the Symptoms of PAD?
The symptoms of PAD, sometimes called peripheral arterial disease, can range from mild to serious. Some people with the disorder "may have no symptoms at all,” says Lee Kirksey, MD, a vascular surgeon at the Cleveland Clinic.
In other cases, it causes problems like:
Claudication. This is leg pain you get when you exercise, usually in your calf or thigh muscles. "Patients typically describe that when they walk a certain distance, they experience cramping, heaviness, or a charley horse," Kirksey says. "When they rest, that discomfort ... goes away, and then when they resume walking a similar distance, they'll experience that discomfort again.”
Wounds and other pain. You could get sores or ulcers on your toes and feet. You might also feel pain in your toes or the front of your foot, even when you're not being active. "Those symptoms indicate that they have very severe peripheral arterial disease,” Kirksey says. People with these symptoms might also notice that their legs and feet are cool, pale, or numb.
Tissue damage. Critical limb ischemia (CLI) is the most serious stage of PAD. This is when the blood flow to your limb is so restricted that sores don’t heal. In this stage, you're at risk of needing an amputation. You'll need surgery to improve the blood flow. Only about 1%-2% of people with PAD reach this stage. Around 30% of them will need an amputation.
How Does PAD Affect Your Sleep?
Based on how serious your PAD is, it can disrupt your sleep in three main ways:
Pain keeps you up. Mild PAD probably won't affect your sleep. But with more severe peripheral artery, you have pain even when you're not moving around. That means it can occur at nighttime and wake you up. Tingling in your foot or toes may also awaken you. Standing up, or hanging your legs over the side of your bed, helps because it forces blood to flow into your lower limbs.
Sleep apnea, a condition linked to PAD, disrupts your sleep. “There's a clear association between (PAD) and obstructive sleep apnea, which is a sleep disorder where people have frequent awakening periods at nighttime,” Kirksey says. "They have periods where they stop breathing or take very small breaths. All those things are disruptive to their sleep.” Apnea is more common in people who are overweight, he says.
When you momentarily stop breathing due to apnea, your oxygen levels dip. That causes inflammation in your body that can affect your heart, blood vessels in your brain, and the arteries leading to your legs and arms, he says. This leads to scarring in your arteries, which can result in blockages and PAD.
Restless legs syndrome, also linked to PAD, wakes you. Around 10%-20% of people with PAD also have this sleep disorder.
“Patients typically describe that they just can't keep their legs still at night. And the movement of their legs typically wakes them up," Kirksey says. "Peripheral arterial disease doesn't necessarily cause restless leg syndrome, but they are associated.”
What Are the Risks?
No matter how it happens, it’s unhealthy to lose sleep over a long period. “Sleep deprivation is associated with coronary artery disease, heart failure, diabetes, an increased risk of heart attack, stroke, and obesity,” Kirksey says.
If serious leg pain is keeping you awake, call your doctor. “That's a medical urgency," he says. "They need to contact their medical provider and have a visit as soon as reasonably possible.”
Also book an appointment if restless legs often interrupt your sleep. “It can be associated with other neurologic disorders, nerve disorders, diabetes, and metabolic and electrolyte disorders,” Kirksey says.
If you have sleep apnea, it might be a good idea to ask your doctor whether you're at risk for PAD, especially if you have family members who've had it.
What Can You Do to Sleep Better With PAD?
If you notice any symptoms of PAD, especially those that keep you awake at night, see your doctor as soon as possible. They can assess your situation and recommend treatment.
You may be able to control a mild case of PAD with exercise. Walking is ideal.
Your doctor may recommend a supervised exercise program. That usually consists of walking on a treadmill, overseen by a nurse or exercise or physical therapist. They'll encourage you to keep going even after you notice leg cramping (claudication).
“Most people’s inclination is to stop walking," Kirksey says. "But the supervised exercise approach suggests that they should push through that discomfort. This helps the muscles develop alternative pathways for blood flow. And that in turn will likely lead to better sleep at night.”