Even 25 years ago, there were few treatments available for people who had rheumatoid arthritis (RA). Back then, the medications doctors could prescribe often caused major side effects and didn’t prevent long-term joint damage. Treatments have come a long way, and researchers are still looking for new ways to get relief from RA symptoms and help prevent long-term health problems like joint damage and disability.
If you or someone you love has RA, here are some key discoveries from the past few years, as well as an update on what researchers are still working hard to figure out.
Anti-Inflammatory Diet Benefits
For years, experts have debated how diet affected RA. Now, two new studies suggest that choosing an anti-inflammatory diet could help ease RA symptoms like joint stiffness, pain, and swelling.
A report published in 2020 in TheAmerican Journal of Clinical Nutrition found that adults with RA who ate an anti-inflammatory diet had less inflammation and joint pain. The anti-inflammatory diet included fatty fish like salmon, whole grains, vegetables, berries, spices, fruits, and low-fat dairy like yogurt, as well as probiotics.
Another study published in 2020 in the journal Nutrients found that a traditional Mediterranean-style diet (little red meat but lots of fatty fish, fruits, and vegetables) helped ease RA symptoms. Researchers also recommended limiting sweetened drinks, salt, and alcohol.
Tai Chi
Your doctor has probably told you that gentle exercise, like yoga and water aerobics, can help you manage and reduce your symptoms. This includes tai chi, is a series of continuous slow-motion exercises that focus on movement and breath -- like a form of moving meditation, In 2018, researchers published a review of seven studies, which showed that many people with RA who did tai chi reported less pain, compared to those who didn’t do that form of exercise. One possible reason? Earlier research shows that tai chi eases stress, which can worsen RA symptoms.
Omega-3 Fatty Acids
It’s important to get most of your nutrients from a balanced diet. If you’re not big on fatty fish, flaxseed, or walnuts, you may be considering adding an omega-3 fatty acid supplement to your daily routine. (It’s always best to check with your doctor before you add any supplement.)
A 2017 study published in JCR: Journal of Clinical of Rheumatology found that taking an omega-3 fatty acid supplement daily helped ease RA symptoms. Researchers reviewed 20 studies on RA and found that 16 of those studies linked supplementing with omega-3 fatty acids to a significant improvement in RA symptoms, including swelling and joint pain. Omega-3 fatty acids play a role in inflammation and may reduce inflammatory chemicals called cytokines.
Stem Cell Therapy
Your body uses stem cells to make other cells with specialized functions. When stem cells are injected into your body, they can create new healthy cells called daughter cells. Experts have been using stem cells to treat medical conditions like Parkinson’s disease and heart disease.
A 2019 study published in Drug Design, Development, and Therapy found that stem cell therapy may help treat RA, too. Researchers discovered that people who couldn’t get relief from RA medications called disease-modifying antirheumatic drugs (DMARDs) or non-steroidal anti-inflammatory drugs (NSAIDs) who got stem cell therapy had significant improvements in their RA symptoms and in their bloodwork for up to 3 years afterward. Those patients didn’t have any major side effects, either.
Keep in mind that researchers say stem cell therapy isn’t a cure for RA, and the FDA hasn’t approved it as an RA treatment. It’s still being studied in clinical trials, while researchers analyze how safe it is and how well it works. If a clinical trial is something you’re interested in, your doctor can help you find one that might be an option to consider -- and help you know what’s involved.
Vagus Nerve Stimulation
This research is still in its early stages, with one small study and no FDA approval yet. The idea is that people with RA who aren’t helped by biologic therapies may get relief from an implantable device that stimulates the vagus nerve. The vagus nerve connects the gut to the brain and plays a role in inflammation, including RA-related inflammation.
A preliminary study on this was published in 2018 in Annals of the Rheumatic Diseases. By studying 14 people, researchers found that more than half of RA patients who got an implanted device that sent electrical impulses to stimulate their vagus nerves had an improvement in RA symptoms.
Janus Kinase (JAK) Inhibitors
One of the biggest advances in RA treatment over the past 2 decades has been the introduction of disease-modifying anti-rheumatic drugs (DMARDs). DMARDs change the way your immune system behaves, which can keep it from attacking your joints and tissues and ease arthritis symptoms. But not all patients get relief from current DMARDs, and there’s a risk of side effects.
Now, newer types of DMARDs called Janus kinase (JAK) inhibitors may offer hope for people who can’t or don’t want to use other DMARDs. Some researchers call JAKs the next generation of RA medications. They’re “small molecule” enzymes that you take by mouth. They send signals from inflammatory chemicals called cytokines, blocking the cytokines and preventing damage. JAKs often have fewer major side effects and are less expensive than some other DMARDs called biologics. There are currently three FDA-approved JAK medications for RA: baricitinib (Olumiant), tofacitinib (Xeljanz XR), and upadacitinib (Rinvoq). Other JAKs are currently in clinical trials for use in RA.
What RA Researchers Still Don’t Know
Autoimmune diseases, including RA, still aren’t fully understood. Some of the mysteries still include:
What causes rheumatoid arthritis. Researchers think rheumatoid arthritis is caused by a mix of things, in your genes and in your environment. What they don’t know is exactly why some people get RA and others don’t. Some people have variations in certain genes that make them more likely to develop RA. But researchers are trying to figure out why those genes get “turned on” in some people and not others. They’re also working to understand how and why certain things in the environment like stress, pollution, smoking, and a poor diet trigger an immune response in the body and raise the odds of getting RA.
When and how to taper DMARDs. Almost all RA medications come with a risk of side effects, and some of them are serious. Because of that, many patients want to taper -- that is, slowly reduce their medications over time, with the goal of going off of them. Some people can successfully taper or go off biologics. Others get painful flares when they try to cut back or quit their medications. Doctors are still trying to figure out how to predict who can successfully taper and why. Experts are hoping that soon, computer programs will help them know which patients will have success weaning off their medications without having flare-ups or long-term damage.
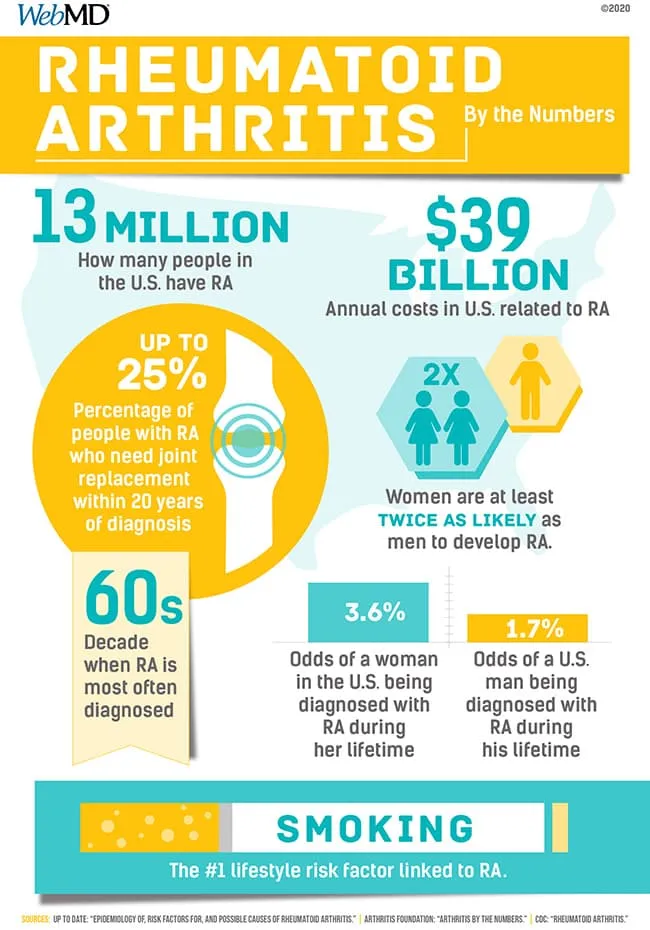
RA Statistics