Experts are seeing more serious tick-borne illnesses -- some of them fatal if not treated right away. Climate change is being blamed for extending tick breeding and biting season. Lyme disease is the most prevalent tick-borne infection in the U.S., with an estimated 300,000 people infected yearly.
In 2019, state and local health departments reported a record number of cases of tick-borne disease to the CDC. Recent statistics reflect a drop in reporting, largely associated with the COVID-19 Pandemic.
There are 10 known vector-borne diseases -- those transmitted by ticks, mosquitoes, and fleas. The vast majority of annual infections -- or 75% -- were caused by ticks.
In August 2019, New York state health officials said a resident died of Powassan virus, a rare but potentially serious disease spread by the black-legged or deer tick. The resident lived in Gardiner and had underlying health conditions, according to the Ulster County Health Department. They said it was the first known case of someone in the state being diagnosed with the disease that summer.
It’s difficult to predict from year to year how many cases of tick-borne diseases will be reported in the U.S. The tiny bugs are now in 50 states, and as a result, more people are at risk every spring, summer, and fall.
Here’s what you need to know about tick-borne illnesses.
Q. Are cases of tick-borne illnesses on the rise?
A. Charts dating back to 1992 show that tick-borne diseases, including Rocky Mountain spotted fever, have risen dramatically. In just one year, from 2016 to 2017, cases rose 23%, CDC figures show. The COVID-19 pandemic is believed to have influenced recent reporting, although not necessarily actual cases.
- Lyme disease: in 2022, 24,611 cases with 42,743 reported in 2017 (Experts believe the annual number is around 300,000, based on surveillance.)
- Anaplasmosis/ehrlichiosis: In 2019, nearly 6000 cases of anaplasmosis and more than 2000 cases of ehrlichiosis
- Rocky Mountain spotted fever: In 2019 - 5207 cases, down from 6,248, in 2017
- Babesiosis: 30,737 during the 2022-2023 outbreak. Tracking started for the disease in 2011 with 1,128 cases.
- Tularemia: 150 cases in 2020
- Powassan virus: 44 cases in 2022
Q. Where are ticks found?
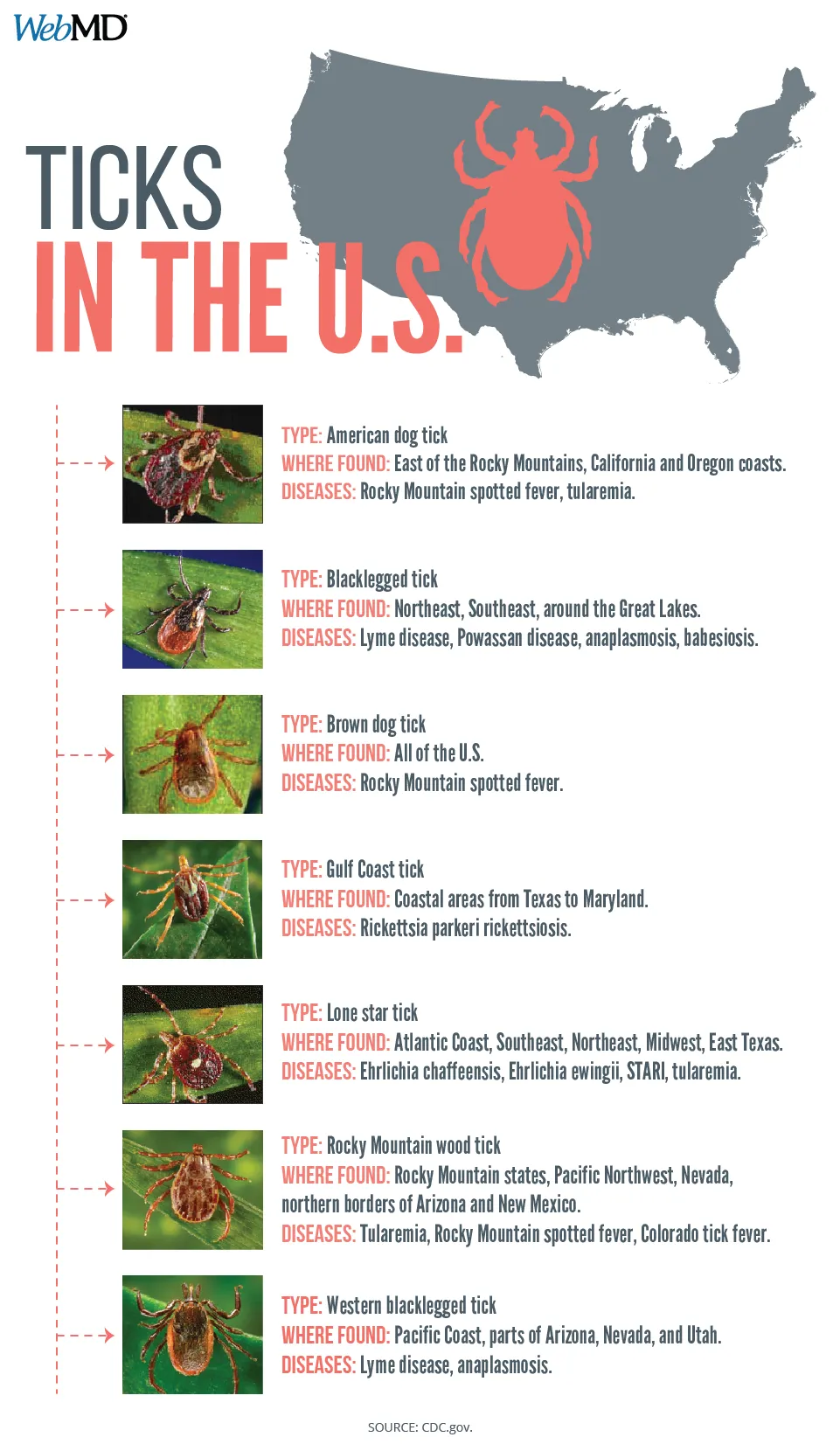
A. The blacklegged tick -- responsible for Lyme disease, the Powassan virus, babesiosis, and anaplasmosis -- is found in every state across the eastern U.S. and into Texas, Oklahoma, Kansas, Nebraska, and the Dakotas. The geographic range of other ticks, including the Lone Star, American dog, brown dog, and Rocky Mountain wood tick, has also expanded throughout North America. They cause Rocky Mountain spotted fever, anaplasmosis, ehrlichiosis, and other infections.
Q. How are tick-borne diseases treated?
A. A simple antibiotic, doxycycline, can be used to snuff out most of the diseases -- if they are recognized and treated early.
Q. How long does a tick have to stick to you to transmit infections?
A. For Rocky Mountain spotted fever, it takes 2 to 96 hours; for Lyme disease, it depends on the tick. One transmits the infection between 4 and 72 hours; the other from 48-96 hours. For anaplasmosis and ehrlichiosis, a tick needs to be attached for 24 to 50 hours. It is unknown how long a tick needs to be attached to transmit Powassan or Heartland virus.
Q. What is the East Asian or longhorned tick?
A. This tick, discovered on a New Jersey sheep farm in late 2017, is known to transmit severe fever with thrombocytopenia syndrome. This potentially fatal disease causes low platelet and low white blood cell counts. It’s now found in Arkansas, Connecticut, Kentucky, Maryland, North Carolina, New Jersey, New York, Pennsylvania, Tennessee, Virginia, and West Virginia.
Q. What is Rocky Mountain spotted fever, and how is it transmitted?
A. You can get this disease from the American dog tick, the brown dog tick, and the Rocky Mountain wood tick. Five states -- North Carolina, Oklahoma, Arkansas, Tennessee, and Missouri -- account for more than 60% of the cases. According to the CDC, about 4,000 to 6,000 cases of tick-borne spotted fevers, including Rocky Mountain spotted fever, are reported each year in this region.
But Native American reservations in southeast Arizona have seen epidemic levels of the disease -- a result of human contact with stray dogs that carry the ticks.
Between 2003 and 2016, public health officials reported more than 360 cases of Rocky Mountain spotted fever in the region, including 21 deaths.
Q. What are symptoms of Rocky Mountain spotted fever?
A. They aren’t much different from the flu -- fever, headache, muscle aches. But within 2-5 days, a rash will begin on your arms and legs and spread to your chest and stomach. At that point, the disease may be doing serious damage to your organs.
Q. How is Rocky Mountain spotted fever treated?
A. Doxycycline is the most effective antibiotic to prevent severe illness and death from Rocky Mountain spotted fever if a patient gets it in the first 5 days of illness. The average time someone dies after showing symptoms is 8 days.
Q: Which other tick-borne diseases are fatal?
A. The death rate from Rocky Mountain spotted fever and anaplasmosis is less than 1%, and it’s about 1% for ehrlichiosis, according to the CDC.
A handful of deaths have been reported from Bourbon, Heartland, and Powassan viruses.
Q. What is the Bourbon virus?
A. The Bourbon virus is likely spread through the bite of a lone star tick or an insect, the CDC says. A handful of cases of the virus have been reported in the Midwest and South, including some that have resulted in death. Symptoms of the virus can include rash, fever, nausea, body aches, tiredness, headache, and vomiting. There is no cure for an infection. Treatment may include IV fluids and pain medications.
Q. What is the Heartland virus?
A. The Heartland virus is caused by the lone star tick. As of November 2022, more than 60 cases have been reported in the Midwest, Northeast, and South, a few of which resulted in death. Symptoms may include fever, headaches, fatigue, muscle aches, and diarrhea. There are no vaccines to prevent this virus or medications to treat it.
Q. What are seed ticks?
A. The phrase "seed ticks" refers to tick larvae. The larvae look like poppy seeds on your skin. Even at this young stage, they can still bite. The bites are commonly painless. The ticks can crawl up your body under clothing and bite you in places that are hard to see.
Q. What is Powassan virus?
A. Unlike some other tick-borne infections, Powassan is a virus. That means antibiotics don’t work to treat it. No antiviral drugs seem to work against it, and there is a high risk of long-term disability and death.
Powassan is rare -- less than 300 cases have been reported since it was first detected in 2002. The numbers have continued to rise as more people come into contact with ticks. The CDC reported 44 cases in 2022.
Q. Where are the most cases of Powassan reported?
A. Cases are concentrated in the northeast U.S. and in the Great Lakes region.
Q. What are the symptoms of Powassan, and are they different from other tick-borne infections?
A. Powassan strikes with fever, chills, muscle aches, and headache, and as the virus progresses, it can lead to seizures and brain and spinal cord inflammation -- conditions that you should go to the hospital for. Unlike other tick-borne diseases, the symptoms of Powassan do not include a rash.
Q. How do you treat the disease?
A. Mainly with supportive care -- painkillers for headache, and hospitalization for people with severe illness. It may include breathing support, intravenous fluids and medications to reduce swelling in the brain. Death is rare and happens in about 10% of the cases that have swelling in the brain, or encephalitis. Other patients end up with long-term memory problems, headaches, and muscle wasting.
Q. Can you get a meat allergy from a tick bite?
A. Scientists aren’t yet sure, but there is data linking something called alpha-gal allergy with tick bites. Alpha-gal is a sugar molecule found in most mammals and some type of ticks. People have allergic reactions after they eat meat from mammals that have it or are exposed to products made from mammals. They may include medications, cosmetics, vaccines, gelatin, and milk products.
Most cases have been reported in the Southeast and Midwest. The Lone Star tick is suspected in cases involving red meat.
Symptoms can be severe and life-threatening. They include rash, hives, difficult breathing, a drop in blood pressure, dizziness or fainting, nausea or vomiting, and severe stomach pain. They usually appear about 3 to 6 hours after eating meat or being exposed to products that have it.
The allergic reaction generally happens within 6 months after the tick bite, usually in someone who had no previous allergies. It’s more common in older adults.
Q. How can I prevent tick bites?
A. Prevention is the only way to avoid infection:
- Limit your exposure to tall grass; walk in the center of trails. Ticks generally latch onto your foot or leg and crawl up your body, often to your head or ears. They don’t jump or fly.
- Remove leaf litter, and clear tall grass and brush around your home and the edge of your yard.
- Use a 3-foot-wide barrier of wood chips or gravel between your yard and wooded areas to keep ticks from coming into your yard.
- Mow your lawn frequently.
- Keep decks, playground equipment, and patios away from trees and the edge of your yard.
- Wear insect repellent with 20% or more DEET, picaridin, or IR3535 on skin that is exposed.
- Treat clothing with the chemical permethrin.
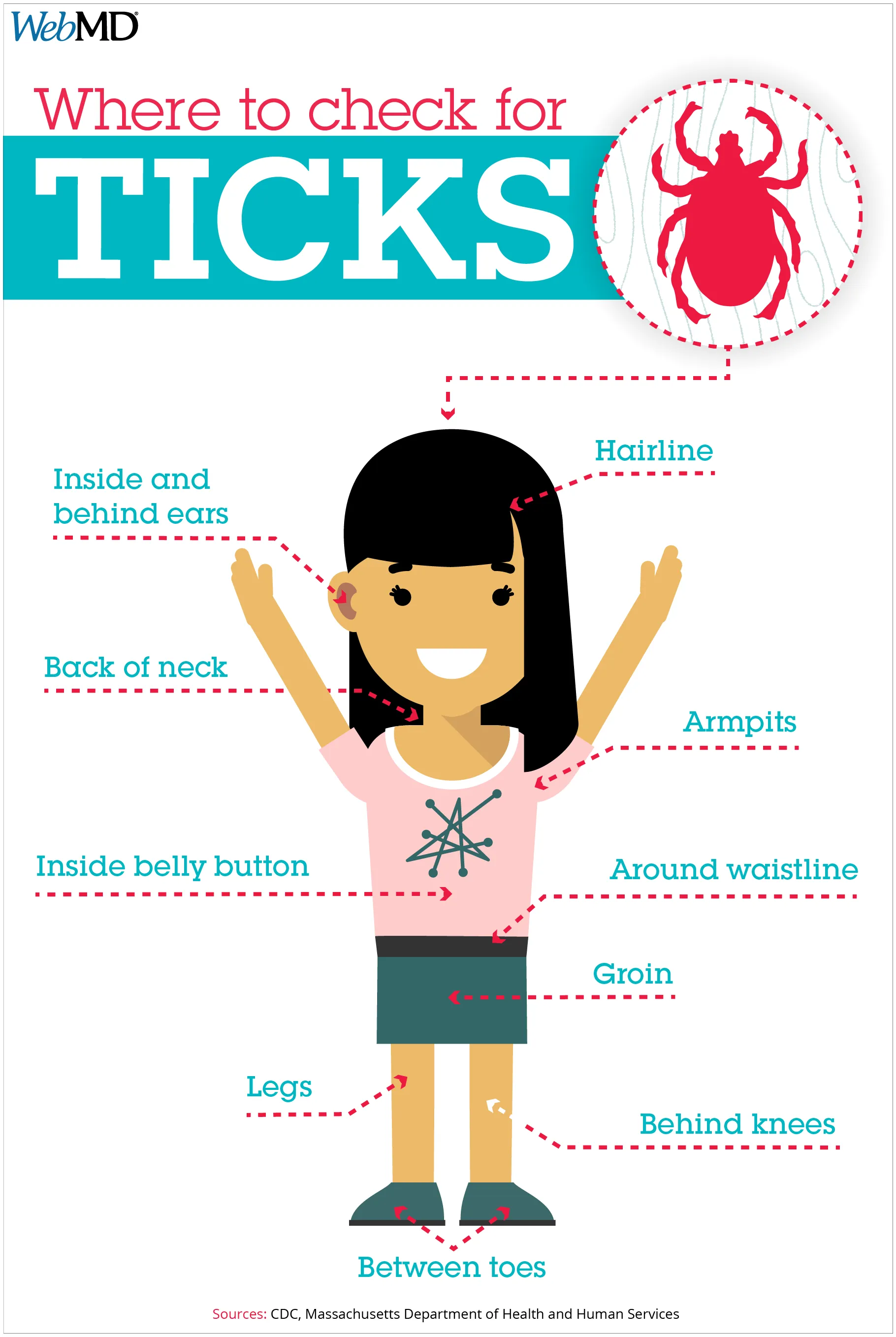
- If you’ve been outside where ticks may live, do a full-body check once you get in, or examine your skin in the shower. Shower as soon as possible after spending time outdoors.
- If you see a tick, remove it with tweezers as close to the skin as possible, pulling it straight out. Dispose of it by flushing it down the toilet or throwing it back outside. Don’t crush it between your fingers. If you suspect it’s an Asian longhorned tick, save it in rubbing alcohol in a jar or a zip-close bag, then contact your local health department.
- Dogs pick up ticks and bring them inside. Check your pet’s skin for ticks, and use tick collars, sprays, shampoos, and medications to prevent ticks.
- Tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors.