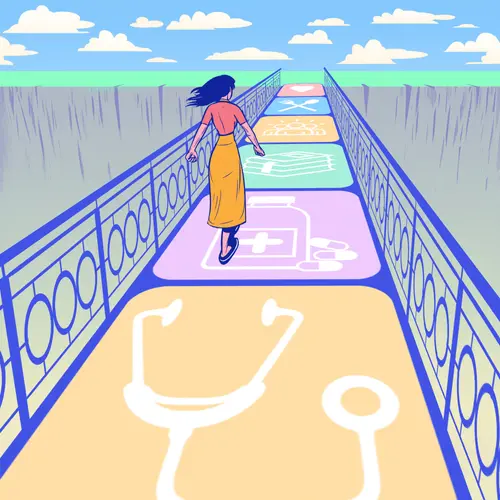
How Do You Qualify for Weight Loss Surgery?
Obesity is a chronic disease that threatens your health and requires long-term management. When lifestyle changes don't work or don't work well enough on their own, you can lose weight with the help of several medications, devices, and surgeries. Weight loss surgery, also called bariatric surgery or metabolic surgery, are operations that help you lose weight by changing your digestive system and appetite.
You may qualify for weight loss surgery if:
- Your body weight is 100 pounds or more above what is considered ideal for your body shape and size.
- You have a body mass index (BMI) of 40 or higher.
- Your BMI is 35 or higher and you have at least one weight-related health condition, such as type 2 diabetes, heart disease, high blood pressure, gallbladder disease, or sleep apnea.
- You have a documented history of unsuccessful weight loss attempts through traditional methods, such as diet and exercise.
- You don't have an alcohol or drug problem.
- You don't have a diagnosed mental disorder.
- You are healthy enough to have the surgery.
Weight loss surgery screening process
Before you get weight loss surgery, you'll go through a thorough screening process. Your doctor will consider your physical and emotional health and whether you’re ready to make permanent lifestyle changes.
You’ll have a nutritional assessment to look at any nutrition deficiencies or unhelpful eating patterns. You’ll likely be tested for eating disorders, depression, and substance use disorder.
Weight loss surgery for teens
Weight loss surgery is usually for adults. But teenagers aged 14 or older may be able to qualify if they meet the criteria above.
Types of Weight Loss Surgeries
There are a few types of weight loss surgery that help with weight loss in different ways. Which one you have depends on your particular weight loss and health needs.
Restrictive surgery. These work by shrinking the size of your stomach and how much you can eat. Reducing the size of the stomach means you can't eat as much and you'll feel fuller faster.
Malabsorptive surgery. This changes how your body digests food so that you don't absorb as many calories. It does this by rerouting how food moves through your digestive system. In some cases, part of your stomach might be removed.
Combination surgery. This combines the effects of restrictive and malabsorptive surgeries.
Adjustable Gastric Banding
Gastric banding is a type of restrictive weight loss surgery.
How it works
Your surgeon uses an inflatable, silicone band called a Lap-Band to squeeze the stomach into two sections: a smaller upper pouch and a larger lower section. The two sections stay connected by a very small channel, which slows down the emptying of the upper pouch. Most people can only eat a half-cup to 1 cup of food at one meal before feeling too full. The food also needs to be soft or well-chewed.
Pros of gastric banding
This operation is simpler to do, minimally invasive, and safer than gastric bypass and other weight loss operations. You don't have to get your stomach or intestines surgically sectioned. You have a smaller scar, faster recovery, and you can have surgery to remove the band if you want to.
How you digest food doesn't change, so you have a lower risk of malnutrition than with other surgeries such as gastric bypass.
You can also get the band adjusted in a doctor's office through a port placed at your skin during surgery. To tighten the band and further reduce your stomach size, your doctor injects more saline solution into the band. To loosen it, your doctor uses a needle to remove liquid from the band.
Cons of gastric banding
If you get gastric banding, you’ll likely have less dramatic and slower weight loss than those who get other surgeries. You can expect to lose about 40%-50% of your excess weight after 2 years compared to the average of 60%-70% after 12 months with other weight loss surgeries.
You also have up to a 50% chance of having complications, such as a blockage that stops you from being able to eat, or problems with the port. Side effects include nausea, vomiting, acid reflux, difficulty swallowing, and constipation. Changing your diet can help. You may also be more likely to regain some of the weight you lose over the years.
Risks of gastric banding
One of the most common side effects of gastric banding is vomiting after you eat too much too quickly. The band might slip out of place, become too loose, or leak. Your risk of needing more surgeries is about 35%. As with any operation, infection is a risk. Although unlikely, some complications can be life-threatening.
Sleeve Gastrectomy
Also called vertical gastric sleeve (VSG) surgery, this is another form of restrictive weight loss surgery. In the operation, your surgeon removes about 80% of your stomach, reducing how much you can eat. What remains is a narrow tube or sleeve about the size of a banana, which connects to your intestines. By removing a part of the stomach that makes hormones that drive hunger, this procedure also decreases your appetite.
Pros of sleeve gastrectomy
A sleeve gastrectomy is one of the safest weight loss surgeries. It's usually done laparoscopically (a minimally invasive procedure done with a small camera as a guide), so you’ll have smaller incisions and quicker healing than with some other surgeries. You can expect to lose about 60% or more of your excess weight in 2 years. If needed, once you’ve lost weight and your health has improved (usually after 12-18 months), you can have a second surgery, such as gastric bypass.
Because it doesn’t affect your intestines, a sleeve gastrectomy doesn't change how your body absorbs food, so you're not likely to fall short on nutrients. And you can eat a wider range of foods than with other procedures.
Cons of sleeve gastrectomy
Unlike gastric banding, a sleeve gastrectomy can’t be reversed.
Risks of sleeve gastrectomy
You have a 15%-20% chance of developing gastroesophageal reflux (GERD). You may develop scar tissue that causes nausea, vomiting, or trouble eating. You may also get gallstones.
Gastric Bypass Surgery (Roux-en-Y Gastric Bypass)
Gastric bypass combines both restrictive and malabsorptive approaches.
In the operation, your surgeon divides the stomach into two parts, sealing off the upper section from the lower. Your doctor then connects your upper stomach directly to the lower section of your small intestine.
Basically, your surgeon creates a shortcut for your food, bypassing part of the stomach and the small intestine. Skipping these parts of the digestive tract means your body absorbs fewer calories and nutrients.
Pros of gastric bypass surgery
Your weight loss tends to be fast and dramatic. You can expect to lose about 70% or more of your excess body weight. Because of the rapid weight loss, conditions affected by obesity — such as diabetes, high blood pressure, high cholesterol, arthritis, infertility, heart disease, cancer, stroke, sleep apnea, and heartburn — often get better quickly.
Gastric bypass also has good long-term results. People can keep an average of 50% of the weight off for 20 years.
Cons of gastric bypass surgery
After the surgery, you won't absorb food the way you used to. That puts you at risk of not getting enough nutrients, which could lead to vitamin and mineral deficiencies. The loss of calcium and iron could lead to osteoporosis and anemia. You'll have to be very careful with your diet and take supplements for the rest of your life.
Another risk of gastric bypass is dumping syndrome, in which food dumps from the stomach into the intestines too quickly before it's been properly digested. About 85% of people who get a gastric bypass have some dumping. Symptoms include nausea, bloating, pain, sweating, weakness, and diarrhea. Dumping is often triggered by eating sugary or high-carbohydrate foods. Adjusting your diet often helps.
Unlike adjustable gastric banding, gastric bypass is more complicated to undo. However, it can be reversed in some cases or converted into sleeve gastrectomy.
Risks of gastric bypass surgery
Because gastric bypass is more complicated, it's riskier. As with most abdominal surgeries, it carries risks such as infection, excessive bleeding, breathing problems, and blood clots. Also, you may get gallstones because of the rapid weight loss. Other risks include bowel obstruction, ulcers, hernias, low blood sugar, stomach perforation, vomiting, and malnutrition.
Biliopancreatic Diversion
In biliopancreatic diversion (BPD), your surgeon removes 80% of your stomach, and then bypasses most of your small intestine. It is less common than other weight loss surgeries. It is typically only recommended if you have a very high BMI or severe weight-related health problems.
Another version of this surgery, called biliopancreatic diversion with a duodenal switch (BPD/DS), is more common now. This surgery keeps the pylorus valve intact, which controls food leaving your stomach. This can help regulate your digestion, which makes malnutrition less common than with a standard biliopancreatic diversion.
Pros of biliopancreatic diversion
Biliopancreatic diversion can result in even greater and faster weight loss than a gastric bypass or sleeve gastrectomy. It is considered one of the most effective weight loss surgeries. It shrinks your stomach so you eat less. This procedure also affects your intestinal hormones in a way that reduces hunger, helps you feel full, and improves blood sugar control.
Cons of biliopancreatic diversion
Biliopancreatic diversion is less common than gastric bypass. One of the reasons is that your risk of not getting enough nutrients is much more serious. It also poses many of the same risks as gastric bypass, including vitamin and mineral deficiencies and dumping syndrome. The duodenal switch operation may lower some of these risks. Frequent diarrhea is a common complication.
Risks of biliopancreatic diversion
This is one of the most complicated and riskiest weight loss surgeries. As with gastric bypass, it poses a fairly high risk of hernias, which will need more surgery to correct. But this risk is lower when your doctor uses minimally invasive procedures (called laparoscopy).
Single Anastomosis Duodeno-Ileal Bypass With Sleeve Gastrectomy (SADI-S)
This is a simpler form of the duodenal switch. Basically, it’s a sleeve gastrectomy followed by a bypass of your small intestine. It has elements of both restrictive and malabsorptive techniques.
Your surgeon first creates a narrow gastric sleeve by removing about 70%-80% of your stomach. They then reroute part of your small intestine, creating two pathways. One carries food from your stomach to the bowel. The other carries bile from your liver into the small intestine.
A smaller stomach means you feel full with less food. And because the food you eat has less time to mix with digestive acids, you absorb fewer calories.
Pros of SADI-S
SADI-S is simpler and safer than the duodenal switch procedure. It has fewer complications than traditional bypass surgeries, and it results in greater weight loss and better control of diabetes. You may lose 80% or more excess body weight. You have a lower chance of developing a hernia than with biliopancreatic diversion. You can have this procedure if you’ve already had a sleeve gastrectomy and aren’t happy with the results.
Cons of SADI-S
You’ll need diet monitoring and nutritional supplements for the rest of your life. You won’t absorb nutrients as well as after other weight loss surgeries such as gastric band or sleeve gastrectomy. You may have bowel movements more often and notice more flatulence.
Risks of SADI-S
Your risk of complications, such as pain, bruising, bleeding, nausea, and leaks at the surgical connection sites, are similar to those of other weight loss procedures. Sleeve gastrectomy can’t be reversed. Since this is a newer procedure, we don’t have as much information on long-term outcomes.
Weight Loss Devices
The gastric balloon and vagal blockade aren’t technically considered weight loss surgeries. But your doctor implants or places one of these devices in your body to help you lose weight.
Gastric balloon/intragastric balloon system
An intragastric balloon is a type of restrictive procedure in which a deflated balloon is placed in your stomach through your mouth. It’s then filled with a saline solution that provides a sense of fullness and reduces hunger. The intragastric balloon won’t work for you if you’ve had previous weight loss surgery or have bowel disease or liver failure.
Pros. There’s no real surgery involved and no hospital stay is needed. The balloon is temporary and stays in place for 6 months. You can lose about 10% of your excess body weight during that time.
Cons. You may have a stomachache, nausea, and vomiting for a few days after the placement of the balloon.
Risks. The FDA in 2018 reported 12 deaths that may have been caused by intragastric balloons (such as from perforation of the stomach or esophagus or the balloon deflating and causing an intestinal blockage). The FDA also received some reports of spontaneous balloon overinflation (either with air or fluid) and pancreatitis caused by the balloon pressing on surrounding organs.
Vagal blockade (vBloc)
An implanted pacemaker-like device sends regular electrical impulses to your vagus nerve, which signals your brain that your stomach is full, so you don’t feel as hungry. The vagus nerve extends from your brain to your stomach. The blockade device is placed under your rib cage and is operated by a remote control that can be adjusted outside your body. You can expect to lose about 25% of your excess body weight.
Pros. Implanting this device is noninvasive. The outpatient procedure may take up to an hour and a half while you’re under general anesthesia. Research shows this is a safe alternative to weight loss surgery.
Cons. You lose less weight than with other procedures. You’ll need to visit your doctor regularly to make sure the device is working correctly or to make any needed adjustments. Side effects can include nausea, vomiting, heartburn, problems swallowing, belching, and chest pain.
Risks. You have a risk of infection or pain at the implantation site. The device has a low rate of serious complications.
Which Weight Loss Surgery Is Best?
The ideal weight loss surgery for you depends on your health and body type.
For instance, if you are very obese, or if you have had abdominal surgery before, simpler surgeries might not be possible. Talk with your doctor about the pros and cons of each procedure.
If possible, go to a medical center that specializes in weight losssurgery. Complications are less likely when surgery is done by experts. Always make sure that your surgeon has had plenty of experience doing the procedure you need.
Takeaways
If you have a significant amount of weight to lose and other medical and lifestyle strategies haven't worked, you may be a candidate for weight loss surgery. These surgeries can help you lose a lot of weight quickly and keep it off, but they also have risks and side effects to consider. For more information and help regarding which weight loss surgery is right for you, speak with your doctor.
Weight Loss Surgery Types FAQs
How safe is weight loss surgery?
Weight loss surgery is generally safe and offers significant health benefits. The risk of death and complications is low. The overall rate of death is around 0.1%, while the chance of major problems is 4%. Your personal risk varies depending on the type of surgery you get, your medical history, how well you follow your dietary restrictions, and your doctor’s skill and experience.
How much weight will I lose 4 months after gastric bypass?
You can expect rapid weight loss in the first 4 months after gastric bypass. After 6-8 weeks, you’ll lose about 10% of your excess body weight. By 12-18 months, that jumps to 65%-80%. Your individual expected weight loss after 4 months varies based on your medical history, genes, and lifestyle factors such as exercise and eating habits.
How painful is bariatric surgery?
You will feel moderate pain over the first week or so. You may feel incision pain and general body aches. Pain medication can help control your discomfort.