What Is Hemoglobin?
Hemoglobin is a protein in red blood cells. It carries oxygen around your body, delivering it to tissues. Hemoglobin also carries carbon dioxide to the lungs so you can breathe it out.
Iron is a part of hemoglobin. It carries oxygen. If your iron is low, your body can’t make hemoglobin or carry enough oxygen to your tissues. Hemoglobin is also the part of blood that gives it a red color.
Hemoglobin structure
Hemoglobin is made up of four protein chains called globins. Two of the globins are called alpha chains and two are called beta chains. Each globin has a compound with an iron molecule in the middle called a heme group. The iron molecule is what binds to oxygen to carry it through your body.
What does hemoglobin do?
Each heme group can hold one oxygen molecule, which means one hemoglobin molecule can hold four oxygen molecules. The alpha and beta chains of hemoglobin are arranged in a special way that helps each oxygen bind efficiently. Once one oxygen molecule binds to a heme group, the structure’s shape changes slightly so that the next oxygen molecule can attach more easily, and so on.
Hemoglobin Levels
The level of hemoglobin your body needs to function well depends on several factors including your age, race, sex, and general health. It can even vary based on where you live. For example, people who live at higher altitudes tend to have a higher range of hemoglobin levels than people who live at lower altitudes.
Normal hemoglobin levels
Hemoglobin is measured in grams per deciliter (gm/dL). Normal levels are different for men and women. The typical ranges are:
Men: 14.0 to 17.5 gm/dL
Women: 12.3 to 15.3 gm/dL
Low hemoglobin
Hemoglobin levels that fall below the normal range can be a sign of certain health conditions such as cancer or anemia. When your hemoglobin is low, your body can’t get enough oxygen to its tissues, and it makes you feel tired and weak.
Low hemoglobin levels may happen because:
- Your body isn’t making enough red blood cells.
- The red blood cells your body is making are dying faster than you can make more.
- You are losing blood from an injury or an illness.
- Your body has trouble absorbing iron.
- You don’t get enough iron, vitamin B12, or vitamin B9 in your diet.
High hemoglobin
If your hemoglobin levels are above normal, it’s usually because your body has had low oxygen levels over time (hypoxia). You might get hypoxia because of:
- Bone marrow disease that increases your red blood cell counts (polycythemia vera)
- Congenital heart disease
- High altitudes
- Failure of the right side of the heart
- Scarring or thickening of the lungs
- Dehydration
High hemoglobin may make you have:
- Headaches
- Blurred or double vision
- Dizziness
- Itching
- Blood clots
Hemoglobin Test
To find out your hemoglobin levels, your doctor can give you a hemoglobin test. They do this by putting a needle into a vein and taking a sample of your blood. Sometimes, they can do the test with blood from a finger stick, or a heel stick in infants. They send the blood sample to a lab for testing.
Often a hemoglobin test is part of a doctor’s routine physical exam. A complete blood count (CBC) is a series of tests on a blood sample that tells your doctor the number of red blood cells, white blood cells, and platelets in your body.
Hemoglobin test at home
You can buy kits that give you hemoglobin level results at home. You take the test by pricking your finger with a small injector. You collect the blood in a test tube which has a solution in it. Then, you shake the blood sample and solution together.
You read the results by comparing the color of the sample to a color card after 2 minutes, which gives you a hemoglobin level estimate.
How to Increase Your Hemoglobin
If you have a low hemoglobin level, your doctor will want to find the underlying cause and treat it, if need be. One common way to raise hemoglobin is to increase the iron in your diet. Specifically, heme iron is a rich source of easily absorbed iron.
Sources of heme iron include:
- Beef
- Chicken
- Tuna
- Pork
- Lamb
- Shrimp
- Halibut
- Oysters
Your body can absorb nonheme sources of iron more easily if you eat sources of vitamin C (such as citrus fruits, tomatoes, kiwi, or broccoli) at the same time. Nonheme sources of iron include:
- Beans
- Nuts
- Cooked spinach, asparagus, and green beans
- Potatoes
- Avocado
- Dried apricots
- Dates
- Raisins
- Whole wheat bread, cereals, and pastas
- Breads fortified with extra iron
- Iron supplements
Anything you cook in iron cookware will also absorb some iron and raise your levels slightly.
What Is an A1c Test?
The hemoglobin A1c test tells you your average level of blood sugar over the past 2-3 months. It's also called HbA1c, the glycated hemoglobin test, or glycohemoglobin. It’s a lot like a baseball player's season batting average. A single game doesn't tell you how a player is performing in their career. Similarly, one day's test results don't give you the complete picture of how your treatment is working.
Your A1c test results help your doctor determine whether you have diabetes. It’s also used to diagnose prediabetes, in which your blood sugar level is higher than it should be but not high enough to qualify as diabetes. If your A1c levels are high enough to indicate either diabetes or prediabetes, but you don’t have symptoms of either, your doctor may order another A1c test on a different day to confirm the diagnosis.
People who have diabetes need this test regularly to see if their levels are staying within range. It can tell if you need to adjust your diabetes medicines.
What is blood sugar (glucose)?
Blood sugar, or blood glucose, provides energy to the cells in your body, allowing them to do their jobs. You get most of your blood sugar from the sugar, fiber, starches, and other carbohydrates in your diet. Your pancreas produces a hormone called insulin, which helps your cells absorb blood sugar to use for energy or to store for later. That process helps keep your blood sugar at a healthy level. But when you have diabetes, this process is disrupted, and without treatment, your blood sugar level remains high.
How the A1c Test Works
The sugar in your blood is called glucose. When glucose builds up in your blood, it binds to the hemoglobin in your red blood cells. The A1c test measures how much glucose is bound.
Red blood cells live for about 3 months, so the test shows the average level of glucose in your blood for the past 3 months.
If your glucose levels have been high over recent weeks, your hemoglobin A1c test result will be higher.
The A1c test can be done in two ways. Let’s look at both.
Blood draw from a vein:
- You'll be seated while a phlebotomist — a health care provider trained to collect blood samples — searches for an easily accessible vein in your arm. A typical spot is your inner arm near the elbow bend.
- After finding and cleansing the area around the vein, they’ll insert a needle and draw blood into a test tube.
- They’ll remove the needle after the tube fills with a sufficient amount of blood.
- The blood sample will then be sent to the lab to be analyzed.
Blood draw from a finger prick:
- You pick the finger that you would like to be used.
- A health care provider will clean and disinfect the chosen finger.
- Next, they’ll prick your finger with a small needle called a lancet.
- They will then squeeze your finger so that a drop of blood forms.
- That drop of blood will be collected into a test container and analyzed.
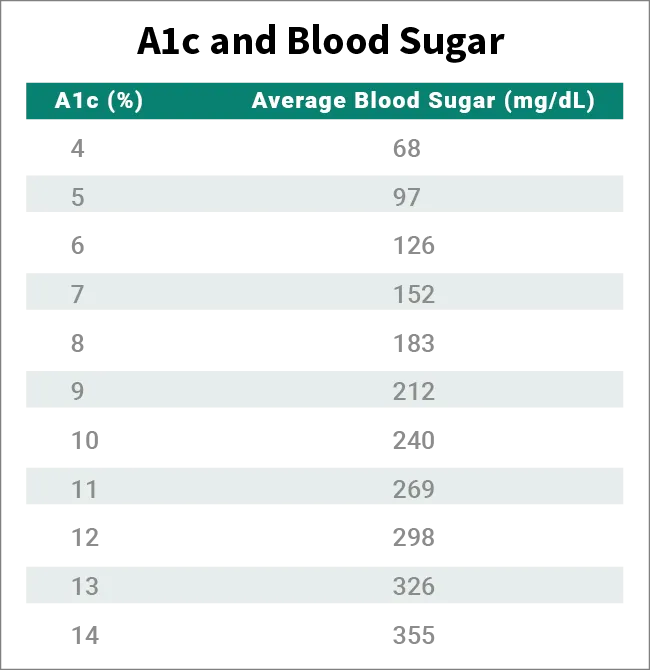
The A1c chart below shows how A1c levels compare with blood sugar levels.
When to Get an A1c Test
There are several reasons why you might need an A1c test, such as if you have symptoms of diabetes. These symptoms include:
- Intense thirst
- More frequent need to pee
- Blurred vision
- Unexpected weight loss
- Feeling tired all the time
- Dry skin
If you don’t have these symptoms, you may get an A1c test to screen for diabetes as part of a routine doctor’s appointment, such as a physical. Several different factors help determine when you should first get your A1c tested and how often the test should be repeated. Keep in mind that different health organizations have different recommendations for when diabetes screening should begin. Let’s look at the CDC guidelines first.
According to the CDC, you should get your A1c tested if:
- You are 45 years or older, even if there’s no reason to suspect you have diabetes.
- You are under 45, overweight or obese, and have at least one prediabetes or diabetes risk factor, such as a family history of diabetes or you are physically active less than three times per week.
How often should you get an A1c test?
Get tested every 3 years if your initial test results were normal but you are:
- Over 45
- Have diabetes risk factors
- Have had gestational diabetes (a type of diabetes that can develop during pregnancy)
If your initial results indicate prediabetes, get tested every 1-2 years or as often as your doctor recommends. Talk to your doctor about lifestyle changes you can make so that you don’t go on to develop diabetes.
If you test positive for prediabetes or diabetes but don’t have symptoms, your doctor will test you again on a different day to confirm the results.
Once your doctor confirms your diagnosis, you’ll get an A1c test twice a year or more. Your testing schedule depends on different factors, such as changes made to your medications, other underlying health conditions, and how well-managed your diabetes is. For example, if you struggle to keep your blood sugar in the healthy range, you may need an A1c test four times a year.
Some health organizations advise that you should start screening for diabetes earlier than age 45. The American Diabetes Association (ADA) recommends the following:
- You should begin screening for diabetes no later than age 35.
- You should begin screening now, whatever your age, if you are overweight, obese, or have other diabetes risk factors.
If your test results are normal, the ADA advises that the test should be repeated every 3 years. Your doctor may recommend screening more often if you have symptoms of diabetes or your risk of diabetes goes up (for example, if you gain weight).
Diabetes screening may be done with an A1c test or another blood test that measures your blood sugar. Because the A1c does not require fasting, it’s considered more convenient than the others. Your doctor will decide which test is best for you.
How to Prepare for an A1c Test
This one’s easy. You don’t need to do anything to prepare for your A1c test.
Do I need to fast for an A1C test?
No, the test doesn't require fasting beforehand, so you’re free to eat and drink normally. But if you have other blood tests scheduled at the same time, they may require special prep. Check with your doctor.
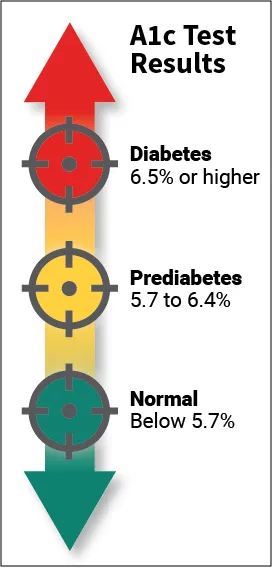
A1c Levels
For people without diabetes, the normal range for the HbA1c level is between 4% and 5.6%. If your levels are in the range of 5.7%-6.4%, it means you have prediabetes and a higher chance of getting diabetes. Levels of 6.5% or higher mean you have diabetes.
What’s a dangerous level of A1C?
If your A1c climbs above 9%, your risk of serious diabetes complications goes up. These complications include:
- Vision loss or blindness
- Kidney failure
- Diabetic neuropathy, or nerve damage, which most commonly affects your hands, feet, arms, and legs
- Heart disease
- Stroke
- Gastroparesis, or paralysis of the stomach, in which your stomach cannot properly digest food
|
How to Lower A1c Levels
The target A1c level for people with diabetes is usually less than 7%. The higher the hemoglobin A1c, the higher your risk of having complications related to diabetes. Someone who has had untreated diabetes for a long time might have a level above 8%.
If you have diabetes and your level is above your target, your doctor may change your treatment plan to get your level down.
A combination of diet, exercise, and medication can help you get an optimal A1c level. If you do use insulin or blood sugar-lowering drugs, your doctor will determine the best dose and schedule to manage your blood sugar level. However, changes to your diet and exercise habits may affect how much diabetes medication you need because both influence your blood sugar level. Here are some tips to help you eat well and exercise safely.
Diet
The foods you eat affect your blood sugar level, so you have to plan carefully. This involves:
Moderating carbohydrates. Carbs are usually the leading culprit behind blood sugar boosts. Knowing exactly how much you’ll consume helps manage your blood sugar level and, if you use insulin, it helps you calculate your dose.
Knowing the proper portion size. Figure out the right portion for the foods you plan to eat, then measure them as precisely as you can.
Eating balanced meals. Your plate should combine protein, carbs, and fat from healthy sources such as fruits, vegetables, and other foods that are good for you. Talk to your doctor or a diabetes dietitian about meal planning and how to coordinate your meals with your diabetes medications.
Skipping sugary drinks. These provide no nutrition but spike your blood sugar. Avoid them except when you need to quickly recover from low blood sugar.
Exercise
Your body burns blood sugar for fuel when you work out, and regular exercise helps insulin do its job of managing the blood sugar in your body. Vigorous workouts provide the most benefits, but lighter physical activities, such as walking, gardening, and simply being on your feet rather than the couch, also help. Aim for at least 30 minutes a day on at least 5 days a week. Here are some tips:
Get advice. Talk to your doctor before you start a new exercise program. Together, you can come up with a plan that will be both beneficial and safe.
Set a schedule. Exercise impacts your blood sugar, so you should coordinate it with both your meal times and medication schedule. Your doctor can help you set an effective schedule as well as tell you what blood sugar level you should target.
Check your levels. Exercise can lower your blood sugar, but it's crucial to prevent it from dropping too low. Check your blood sugar before, during, and after you exercise. This is particularly important if you are on insulin or any blood sugar-lowering drugs. You may need a small snack before you work out or while you exercise to prevent low blood sugar. Finally, know the signs of low blood sugar: feeling shaky, weak, tired, hungry, lightheaded, irritable, anxious, or confused. You may need to alter your insulin or medication in order to account for the impact that exercise can have on your blood sugar level.
Drink water. You need to stay hydrated while you are active to prevent a rise in your blood sugar level.
How much can your A1c drop in 3 months?
The answer to that question is different for everyone and depends on lots of factors. Making healthy changes to your diet and adding regular exercise to your routine are two major components of getting your A1c down — and keeping it down.
A reasonable goal is to maintain your A1c between 7% and 8%. Some people can bring it down even further, to 6.5% or lower. Your doctor can help you decide the best goal for you to set.
What Can Affect Your A1c Results
A lot of factors can throw off the accuracy of your A1c results. One of these is the type of hemoglobin you have. This is determined by your genes. Hemoglobin A is the most common type, but you may have another type — called a hemoglobin variant — if you are Hispanic or of West African or Southeast Asian descent. Having a hemoglobin variant may affect your test results.
A blood test can be done to learn what type of hemoglobin you have. This is important to know so that the lab accurately analyzes your A1c.
There are other factors as well that can make your A1c results appear lower or higher than they actually are.
Falsely low results
Some health conditions and other factors can cause your A1c test results to be lower than they actually are. They include:
- Alcohol use disorder
- Blood transfusion
- Chronic kidney failure and some of its treatments
- Bleeding
- Being pregnant
- Cirrhosis of the liver
- Sickle cell anemia and hemolytic anemia
- High-altitude living
- Taking an iron supplement
Falsely high results
An artificially high A1c test result can be caused by any of the following factors:
- Certain types of anemia, including iron-deficiency anemia
- Drugs that suppress your immune system
- High triglycerides, a type of fat that circulates in your bloodstream
- An organ transplant
- Thalassemia, a blood disorder that keeps your body from producing a normal amount of hemoglobin and red blood cells
- Vitamin B12 deficiency
How Often Do You Need an A1c Test?
Your doctor probably will have you take the A1c test as soon as you’re diagnosed with diabetes. You’ll also have the test if your doctor thinks you may get diabetes. The test will set a baseline level so you can see how well you’re controlling your blood sugar.
How often you’ll need the test after that depends on several things, such as:
- The type of diabetes you have
- Your blood sugar control
- Your treatment plan
You’ll probably get tested once a year if you have prediabetes, which means you have a strong chance of developing diabetes.
You may get tested twice each year if you have type 2 diabetes, you don't use insulin, and your blood sugar level is usually in your target range.
You could get it three or four times each year if you have type 1 diabetes.
You may also need the test more often if your diabetes plan changes or if you start a new medicine.
A1c Test at Home
You don’t have to go to your doctor’s office to take your A1c test. You can do it at home. For some people, such as those who live in rural areas far from a health care provider, at-home tests offer a welcome alternative to driving to the doctor’s office. Their use greatly expanded during the COVID-19 pandemic as telemedicine grew in popularity.
Research does suggest, however, that at least some at-home A1c tests are not quite as accurate as the tests done in your doctor’s office. Ask your doctor which tests are the most reliable.
Some at-home A1c tests, called rapid tests, will give you results within a few minutes, while others require you to mail your blood sample to a lab for analysis. Results for mail-in tests take at least a few days to become available.
Below are some basic instructions so you know what to expect. Each test is going to be somewhat different from the others, so be sure to carefully read and follow the instructions that come with your kit.
For rapid tests:
- Wash and dry your hands before testing.
- Prick your finger with the lancet, or needle, to draw blood.
- Use the collector device included in your test kit to collect a sample.
- Insert the collector into the shaker device, which holds the testing solution.
- Shake several times to combine your blood sample with the testing solution.
- Insert the shaker into the analyzer included in your test kit.
- Wait for 5 minutes, then check the results.
For mail-in tests:
- Wash your hands with warm water.
- Select the finger you’ll use.
- Clean your finger with the alcohol swab included in your kit and let it dry.
- Pierce your finger with the lancet included in your kit.
- Massage, but don’t squeeze, your finger to encourage blood to flow.
- Tap the blood drops against the inside of the collection tube included with your kit and fill to the line marked on the side.
- Close the tube firmly and shake it up and down 10 times to thoroughly mix the sample.
- Place the tube in the biohazard bag included in your kit, seal it, and then place the bag in the mailing envelope provided.
- Mail it back the same day.
Some mail-in kits collect blood on a card rather than in a tube. The instructions provided in your kit will walk you through the process.
A1c Test Risks
As with other blood tests, the A1c test presents no real risks. The spot where the blood was drawn may become tender or bruised, but this typically clears up quickly.
Limitations of A1c Tests
The A1c test is a valuable tool for diagnosing and managing diabetes, but it’s not perfect. As detailed above, it’s not always accurate. Another limitation is that it does not tell you how your blood sugar level fluctuates throughout the day, week, or month. Such fluctuations are particularly common in type 1 diabetes. Because the test only gives an average blood sugar level over the previous 3 months, your result could be the same whether your blood sugar fluctuates a lot or stays steady.
Why is that important? Your goal is to keep your blood sugar level in your desired range as much as possible. Your "time in range" numbers provide a better picture of how well you manage your diabetes day to day and week to week. The A1c was not designed to do that. For that, you need a continuous glucose monitor, which tracks your glucose level 24/7.
Takeaways
The A1c test is a blood test that measures your blood sugar level over the previous 3 months. It plays an important part in diagnosing and managing diabetes. If you have diabetes, expect to take an A1c test at least twice a year. But keep in mind that some health conditions and other factors can affect its accuracy. You may need to use additional means, such as a continuous glucose monitor, to keep close track of your blood sugar level from day to day.
Hemoglobin A1c FAQs
What does a hemoglobin A1c test measure?
This test measures your average blood sugar (aka blood glucose) level over the previous 3 months. It is used to diagnose and manage diabetes.
What is a normal A1c range by age?
A1c tests calculate the percentage of blood sugar in your bloodstream. The normal range, meaning you don’t have diabetes, is below 5.7%. That normal range remains the same no matter your age.
Does a high A1c level mean I have diabetes?
Maybe. If you have no symptoms of diabetes when you take the test, your doctor will schedule a follow-up A1c test to confirm the result. Also, several health conditions and other factors can make the A1c test less accurate, potentially causing falsely high or falsely low results. Your doctor should consider these factors when evaluating your A1c test result.
What happens if your hemoglobin is low?
Low levels of hemoglobin keep your body from delivering enough oxygen to tissues. As a result, you feel tired and weak, and your body can’t function like it should.
What happens if your hemoglobin is high?
High levels of hemoglobin thicken your blood. This keeps it from flowing as easily, which means your organs can’t get the amount of oxygen they need. You may get headaches, dizziness, blurred or double vision, itching, and blood clots.
Is high or low hemoglobin bad?
Your hemoglobin levels give your doctor important information about the health of your red blood cells. Both high and low levels of hemoglobin can be signs that your tissues and organs aren’t getting the oxygen they need. They can also indicate underlying problems.
Is high hemoglobin something to worry about?
Some causes of high hemoglobin can be serious, such as bone marrow disease, congenital heart disease, heart failure, and scarred lungs. But other factors that can cause it include time spent at a high altitude and dehydration. Your doctor can test you for conditions that may be raising your hemoglobin levels.
What causes hemoglobin to be a little high?
Most often, high hemoglobin happens because your blood oxygen levels have been low for some time. This might be because of an illness or injury. Your doctor will examine you and may do tests to find out what’s behind your high hemoglobin levels.