Uses
This medication is used to treat high pressure inside the eye due to certain types of glaucoma. Lowering high pressure inside the eye helps to prevent blindness, vision loss, and nerve damage. Methazolamide belongs to a class of drugs known as carbonic anhydrase inhibitors. It works by decreasing the production of fluid inside the eye.
How to use Methazolamide
Take this medication by mouth as directed by your doctor, usually 2 or 3 times a day. This medication may be taken with food if stomach upset occurs. To reduce your risk of certain side effects (kidney stones), drink plenty of fluids unless otherwise directed by your doctor.
The dosage is based on your medical condition and response to treatment.
Use this medication regularly to get the most benefit from it. To help you remember, take it at the same times each day. Keep taking this medication even if you feel well. Most people with glaucoma or high pressure in the eye(s) do not feel sick.
Side Effects
Nausea, loss of appetite, change in taste, vomiting, diarrhea, frequent urination, dizziness, drowsiness, or tiredness may occur as your body adjusts to the medication. If any of these effects last or get worse, tell your doctor or pharmacist promptly.
Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.
Tell your doctor right away if you have any serious side effects, including: signs of kidney stones (such as painful urination, fever, chills, pink/bloody urine), signs of infection (such as sore throat that doesn't go away, fever, chills), easy bleeding/bruising, numbness or tingling of hands/feet, ringing in the ears.
Get medical help right away if you have any very serious side effects, including: signs of liver problems (such as nausea/vomiting that doesn't stop, loss of appetite, stomach/abdominal pain, yellowing eyes/skin, dark urine), confusion, fast/pounding heartbeat, seizures.
A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.
This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.
In the US -
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.
In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
Precautions
Before taking methazolamide, tell your doctor or pharmacist if you are allergic to it; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.
Before using this medication, tell your doctor or pharmacist your medical history, especially of: adrenal gland problems (such as Addison's disease), liver disease (such as cirrhosis), breathing problems (such as chronic obstructive pulmonary disease-COPD, emphysema, lung infection), diabetes, gout, kidney problems (such as history of kidney stones), untreated mineral imbalance (such as low sodium/potassium, hyperchloremic acidosis), overactive thyroid (hyperthyroidism).
This drug may make you dizzy or drowsy. Alcohol or marijuana (cannabis) can make you more dizzy or drowsy. Do not drive, use machinery, or do anything that needs alertness until you can do it safely. Limit alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).
This medication may make you more sensitive to the sun. Limit your time in the sun. Avoid tanning booths and sunlamps. Use sunscreen and wear protective clothing when outdoors. Tell your doctor right away if you get sunburned or have skin blisters/redness.
Before having surgery, tell your doctor or dentist about all the products you use (such as prescription drugs, nonprescription drugs, and herbal products).
During pregnancy, this medication should be used only when clearly needed. Discuss the risks and benefits with your doctor.
It is unknown if this medication passes into breast milk. Consult your doctor before breastfeeding.
Interactions
Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (such as prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.
Some products that may interact with this drug are: memantine, methenamine.
Check the labels on all your medicines because they may contain aspirin or aspirin-like drugs (salicylates), which can cause serious side effects if taken in large doses with this medication. However, if your doctor has told you to take low-dose aspirin to prevent heart attack or stroke (usually 81-162 milligrams a day), you should keep taking the aspirin unless your doctor tells you not to. Ask your doctor or pharmacist for more details.
This medication may interfere with certain lab tests, possibly causing false test results. Make sure lab personnel and all your doctors know you use this drug.
Overdose
If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call 1-800-222-1222. Canada residents can call 1-844-764-7669.
Do not share this medication with others.
Lab and/or medical tests (such as potassium level, complete blood count, liver function) should be done while you are taking this medication. Keep all medical and lab appointments. Consult your doctor for more details.
If you miss a dose, take it as soon as you remember. If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
Store at room temperature away from light and moisture. Do not store in the bathroom. Keep all medications away from children and pets.
Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
Images

methazolamide 25 mg tablet
Color: whiteShape: squareImprint: ANI 240This medicine is a white, square, tablet imprinted with "ANI" and "240".

methazolamide 50 mg tablet
Color: whiteShape: roundImprint: ANI 241This medicine is a white, square, tablet imprinted with "ANI" and "240".

methazolamide 25 mg tablet
Color: whiteShape: roundImprint: ZEN 25This medicine is a white, square, tablet imprinted with "ANI" and "240".

methazolamide 50 mg tablet
Color: whiteShape: roundImprint: EFF 2 0This medicine is a white, square, tablet imprinted with "ANI" and "240".
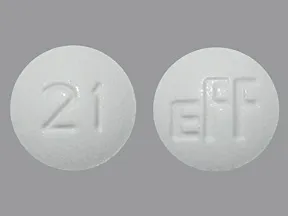
methazolamide 25 mg tablet
Color: whiteShape: roundImprint: 21 EFFThis medicine is a white, square, tablet imprinted with "ANI" and "240".
Are you currently using Methazolamide?
This survey is being conducted by the WebMD marketing sciences department.
Selected from data included with permission and copyrighted by First Databank, Inc. This copyrighted material has been downloaded from a licensed data provider and is not for distribution, except as may be authorized by the applicable terms of use.
CONDITIONS OF USE: The information in this database is intended to supplement, not substitute for, the expertise and judgment of healthcare professionals. The information is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects, nor should it be construed to indicate that use of a particular drug is safe, appropriate or effective for you or anyone else. A healthcare professional should be consulted before taking any drug, changing any diet or commencing or discontinuing any course of treatment.