What Are Varicose Veins?
Varicose veins are bulging, sometimes bluish veins that look like cords running just beneath the surface of your skin. They usually affect the legs, ankles, and feet.
Varicose veins that are visibly swollen, twisted, and sometimes surrounded by patches of flooded capillaries (or small blood vessels) known as spider veins are considered superficial varicose veins. They may cause swollen ankles, itchy skin, and aching in the affected area. Superficial varicose veins can be painful but are usually harmless.
Along with veins that run along the surface of your skin, your legs have interior, or deep, veins. Sometimes, an interior leg vein becomes varicose (abnormally swollen or enlarged). Such deep varicose veins are usually not visible, but they can cause swelling or aching throughout the leg and may serve as sites where blood clots can form.
Varicose veins are a relatively common condition. For many people, they are a family trait. Women are at least twice as likely as men to develop them. In the U.S. alone, they affect up to 35% of people.
Spider veins vs. varicose veins
Spider veins are smaller than varicose veins and don’t bulge out. They look like spider webs or tree branches, and they are red, blue, or purple. Unlike varicose veins, spider veins may also appear on your face.
Both varicose and spider veins are damaged blood vessels, but spider veins are not actually veins — they are capillaries, venules, and arterioles, which are smaller blood vessels. Spider veins rarely cause pain or other symptoms beyond their appearance.
Varicose Veins Causes
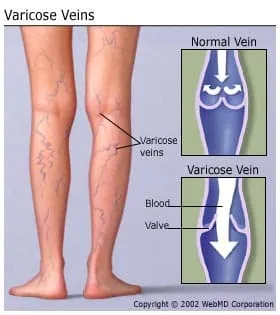
To help move oxygen-rich blood from the lungs to all parts of the body, your arteries have thick layers of muscle or elastic tissue. To push blood back to your heart, your veins rely mainly on surrounding muscles and a network of one-way valves. As blood flows through a vein, the cup-like valves open to allow blood through, then close to prevent backflow.
In varicose veins, the valves do not work properly, allowing blood to pool in the vein and making it difficult for the muscles to push the blood "uphill." Instead of flowing from one valve to the next, the blood continues to pool in the vein, increasing pressure in the veins and the odds of buildup, causing the vein to bulge and twist. Because superficial veins have less muscle support than deep veins, they are more likely to become varicose.
Any condition that puts too much pressure on the legs or abdomen can lead to varicose veins. The most common things that bring about pressure are pregnancy, obesity, and standing for long periods of time. Chronic constipation and -- in rare cases, tumors -- also can cause varicose veins. Not being active also may lead to varicosity because muscles that are out of condition offer poor blood-pumping action.
The odds of getting varicose veins also increase with age, as veins weaken when you get older. A previous leg injury may damage the valves in a vein, resulting in becoming varicose. Your family history also plays a role, so if other family members have varicose veins, there is a greater chance you will, too. Contrary to popular belief, sitting with crossed legs will not cause varicose veins, although it can impact an existing condition.
Varicose veins in pregnancy
During pregnancy, the volume of blood in your body increases to support the growing baby. This can enlarge the veins in the legs.
The uterus puts pressure on your veins during pregnancy, which can also lead to varicose veins, sometimes around the vagina and buttocks. After childbirth, varicose veins may or may not go away.
The changes in hormones during pregnancy also may relax the vein walls, contributing to varicose veins.
Varicose Veins Risk Factors
Certain things -- some of which you can control and some of which you can’t -- increase the chances that you’ll get varicose veins. They include:
- Pregnancy. Varicose veins usually improve 3 months to a year after delivery.
- Family history. You are more likely to have varicose veins if they run in your family.
- Obesity. Being overweight puts extra pressure on your veins.
- Older age. Valves in the veins weaken because of wear and tear as you age. Your veins start to lose elasticity, so vein walls and valves don’t work as well.
- Your sex. Women are four times more likely than men to get varicose veins.
- Pregnancy. Women often get varicose veins for the first time during pregnancy. They usually improve 3 months to a year after delivery.
- Lack of exercise
- Prolonged standing or sitting. Standing or sitting for long periods decreases circulation.
- Vascular diseases. Blood vessel diseases such as deep vein thrombosis (DVT) can increase your risk for varicose veins.
- Smoking
- Taking birth control pills or hormone replacement therapy
- Injury to your leg
Varicose Veins Stages
Varicose veins may not be cause for concern if they're only cosmetic. But if they are serious and go untreated, they may get worse. Without treatment, they may cause ulcers, bleeding, and skin discoloration.
Sometimes, varicose veins can develop into more serious conditions, such as chronic venous insufficiency, which means the veins in your legs are damaged and don’t work properly.
Venous diseases are classified by a CEAP (Clinical, Etiological, Anatomical, and Pathophysiological) clinical score, which is a range of categories that note the level of certain vein problems. The categories are:
- C0: No visible signs of venous disease
- C1: Telangiectasia (also known as spider veins) or reticular veins (similar to spider veins but larger)
- C2: Varicose veins
- C3: Edema, which is swelling due to fluid trapped in the tissues of your body
- C4: Changes in skin and subcutaneous tissue (tissue under the skin)
- C4a: Pigmentation or eczema
- C4b: Lipodermatosclerosis (inflammation of fat under the skin) or atrophie blanche (scarring on the skin that happens with delayed healing and poor blood supply)
- C5: Healed venous ulcer (wound from issues with vein and blood flow that's healed)
- C6: Active venous ulcer (wound from issues with vein function and blood flow that's still present)
Varicose Veins Symptoms
Some symptoms of varicose veins are just cosmetic, but others involve pain or discomfort.
Early-stage varicose veins symptoms
Symptoms may include:
- Bulging, bluish veins
- Skin color changes around the veins
- Swelling in the legs
- Aching pain in the legs
- A heavy feeling in the legs and feet
- Nighttime leg cramps
- An itching or burning feeling around the veins
- Pain that worsens after prolonged sitting or standing
Other varicose vein symptoms
Other symptoms include:
- Prominent dark purple or blue blood vessels, visible on the thighs and calves
- Aching, tender, heavy, or sore legs, often accompanied by swelling in the ankles or feet after standing for a long time
Do varicose veins hurt?
Varicose veins may or may not hurt. Sometimes, the only symptoms are the way the veins look.
Varicose veins and bruising
If you have varicose veins, your legs may bruise easily because of the enlarged veins near the surface of your skin.
Varicose Veins Diagnosis
To determine whether you have varicose veins, your healthcare provider will examine you and ask about your symptoms. They may use ultrasound to see how the blood is flowing through the valves in your veins.
Varicose Veins Treatment
The treatment for varicose veins can range from simple home remedies to surgery.
Varicose veins socks
Wearing compression stockings, or compression socks, can help because they squeeze your legs and help your veins and leg muscles circulate blood.
These can help by squeezing the veins to prevent blood from pooling. They work best if you wear them every day. You can try a low-tech version by wearing support pantyhose, which offer a similar compression effect.
You can buy compression stockings over the counter at drugstores. Or your doctor may give you a prescription for compression stockings that you can get at a medical supply store or pharmacy. A trained worker will fit the stockings specifically for you. This type gives you the most support.
Elevating your legs
Raising your feet above the level of your heart a few times a day can reduce swelling and help relieve symptoms.
Varicose veins cream
Some creams and lotions claim to help treat varicose veins, but their effectiveness has not been proven.
Varicose veins surgery
A surgery called vein ligation or vein stripping involves tying off and removing varicose veins. This treatment may be used when less invasive procedures don't work.
For more serious varicose veins, your doctor may recommend endoscopic vein surgery. This procedure uses a small camera on a tiny tube. Your doctor threads it into your vein through a cut in your skin. They use a surgical device at the end of the tube to close your vein.
You probably won’t need this procedure unless your varicose veins cause severe skin ulcers. If you have endoscopic vein surgery, you can go back to your normal routine within 2 weeks.
Varicose veins laser treatment
With laser treatment, strong bursts of light are directed onto the varicose vein, which makes it fade until you can’t see it. They don’t need to make any cuts or use any needles in this procedure. It’s used mostly for smaller varicose veins.
Another procedure called endovenous ablation uses laser or radiofrequency energy to heat the inside of the varicose vein and close it off.
You’ll be awake during the procedure. First, they’ll numb the area around the vein. Then, they’ll make a small cut in your skin and insert a thin tube. The tube has a device that uses a laser or radio wave to create heat. That closes the vein. Most people feel only the injection of the numbing agent.
You may go home later in the day. Your leg will be wrapped in a compression bandage after the procedure.
Other treatments for varicose veins
You can make lifestyle changes that may keep your varicose veins from getting worse, stop new ones from forming, and reduce your pain. However, there are other things you can try, and they can usually be done in a doctor’s office.
There are ways to close off a varicose vein. When your doctor does this through a procedure, your blood flow simply shifts to other veins. After the vein is closed, it fades away. There are also procedures to remove varicose veins. The procedures that can close off or remove varicose veins include:
Sclerotherapy. Sclerotherapy is the most common treatment for varicose veins. You can have this procedure done in a doctor’s office. Your doctor injects a solution into the vein that causes it to scar. This forces blood to change routes, going through healthier veins instead. Your collapsed vein is reabsorbed into the surrounding tissue.
You may need several treatments -- usually 4-6 weeks apart -- to completely close off a vein. You won’t need anything to numb you, and the only discomfort you’ll feel will be the sensation of small needle pricks from the injections. You’ll need to wear compression stockings for a few weeks after each procedure.
Microsclerotherapy. It’s similar to sclerotherapy but uses a smaller needle to treat smaller varicose veins.
Ambulatory phlebectomy. This is a less complicated procedure, and it is used to remove varicose veins close to the surface of your skin. Your doctor will numb the area and remove veins through small cuts. You remain awake and generally can go home the same day.
Vein stripping and ligation. This is the solution for the most serious cases. You will be given general anesthesia so that you will not be awake during the procedure.
Your doctor will make cuts in your skin, tie off the veins, and remove them. If possible, the doctor will try to leave what’s called the saphenous vein, just in case you need it later for a heart bypass surgery. You might go home the same day you have the surgery. Recovery time ranges from 1 to 4 weeks.
After your procedure
You might feel side effects after your treatment. The most common ones are swelling, bruising, changes in skin color, and pain.
You’re more likely to have serious side effects if you’ve had vein stripping and ligation. Although they’re rare, complications can include blood clots, severe pain, infection, and scarring.
The doctor may wrap your legs in elastic bandages after your procedure and have you wear compression stockings for a certain amount of time.
When you get home, follow instructions about exercising even though you’re sore. Inactivity raises the chance that you’ll develop a dangerous blood clot.
No matter what procedure you choose, it can only treat existing varicose veins. New ones may develop, but you can take the following steps to limit them:
- Watch your weight.
- Exercise regularly.
- Raise your feet when you sit.
- Don’t cross your legs when you sit.
- Don’t wear tight clothes.
Varicose veins treatment cost
The cost of varicose vein treatments varies widely, from $10 to $100 for compression stockings to thousands of dollars for surgery. Your health insurance may or may not cover the cost of treatment. Some insurers cover treatment if it's considered medically necessary but not if it's considered cosmetic.
When to Worry About Varicose Veins
If your symptoms are mild, remedies such as compression socks may be all you need. But if your symptoms are severe or the appearance of your varicose veins is distressing to you, you should see a health care provider. You should also contact your doctor if:
- Your symptoms keep your body from functioning normally, or the skin over your varicose veins becomes flaky, ulcerated, discolored, or prone to bleeding -- you could be developing stasis dermatitis. If left untreated, stasis dermatitis can lead to skin infections and chronic leg ulcers.
- You have red, warm, and tender varicose veins. This may be a sign of phlebitis, which is caused by a blood clot in the vein.
You have injured a varicose vein. Control the resulting burst of blood with direct compression and leg elevation. Have your veins evaluated by a vein specialist, as this can be a potentially serious complication.
If the symptoms of your varicose veins worsen suddenly or you notice bleeding or a sore, you should call your doctor right away.
Are varicose veins dangerous?
Varicose veins typically are not dangerous. Your only symptoms may be what the veins look like. But in some cases, varicose veins can be harmful because they can lead to more serious health problems.
Varicose Veins Complications
Complications of varicose veins are rare, but they can be serious. They include:
Ulcers. On the skin near varicose veins, ulcers (open sores) can form, and they can be painful.
Bleeding. Varicose veins that are close to the skin can burst and cause bleeding.
Blood clots. If you have varicose veins, you may be more likely to develop blood clots, including a type called DVT, which is a blood clot deep inside the body.
Chronic venous insufficiency. Severe varicose veins may be a sign of this condition, which means your veins are unable to pump blood to your heart the way they should.
How to Prevent Varicose Veins
Even though your genetics play a part in your risk for varicose veins, there are things you can do to prevent them:
Exercise regularly. Staying fit is the best way to keep your leg muscles toned, your blood flowing, and your weight under control.
Maintain a healthy weight.If you aren't at a healthy weight or have obesity, losing weight can improve blood flow and ease the pressure on the veins in your legs and feet.
Avoid tight clothing. Tight clothes can cause poor blood flow in the waste, groin, or legs.
Avoid high-heeled shoes. Wearing high heels for long periods can slow down circulation. Flat or low-heeled shoes are better for circulation, as they can improve calf muscle tone.
Move around. Avoid sitting or standing for long periods to boost blood flow. If your daily routine requires you to be on your feet constantly, consider wearing daily support hose or compression stockings. Take breaks to walk around, and stretch and exercise your legs as often as possible to increase circulation and reduce pressure buildup. When you are sitting, try elevating your feet and changing your position often to improve blood flow.
Quit smoking. Studies show that smoking may play a role in forming varicose veins.
If you're pregnant, sleep on your left side rather than your back. This will minimize pressure from the uterus on the veins in your pelvic area. This position will also improve blood flow to the fetus. If you are prone to developing varicose veins, ask your doctor for a prescription for compression stockings.
Living With Varicose Veins
Maintaining a healthy lifestyle and making some changes to your daily routine, as listed above, can help you manage discomfort from varicose veins as well as improve the appearance of varicose veins.
If the appearance of your varicose veins bothers you, talk to your doctor about your treatment options.
Varicose veins exercise
Exercises, such as walking and swimming, help improve blood flow. It works your leg muscles, which can help pump the blood back up toward your heart and prevent it from pooling in your veins.
Other changes you might try include:
- When you sit, don’t cross your legs.
- Reduce the amount of salt in your diet. This can reduce swelling in your legs.
- Talk to your doctor before you start any new activity.
Takeaways
Varicose veins are common, and they may not be bothersome beyond what they look like. But if they cause discomfort, there are things you can do in your daily life to improve blood flow and manage your symptoms. If your varicose veins are painful or severe, it’s a good idea to see your health care provider because varicose veins can lead to more serious problems.
Varicose Veins FAQs
Can you fix varicose veins on your own? You can’t get rid of varicose veins on your own, but if they are not severe, you may be able to manage your symptoms on your own.
How can I stop varicose veins from getting worse? By taking preventive measures such as exercising and wearing compression stockings, you may be able to keep varicose veins from getting worse.
What should you not do with varicose veins? If you have varicose veins, you should avoid being still or seated for long periods of time. It’s important to move around and exercise.
Can you get rid of varicose veins without surgery? In some cases, your health care provider can get rid of varicose veins with treatment other than surgery.

