Cervicitis is inflammation of the cervix -- the lower end of the uterus that opens into the vagina.
Cervicitis is common. It may be caused by a number of factors, including infections, chemical or physical irritations, and allergies.
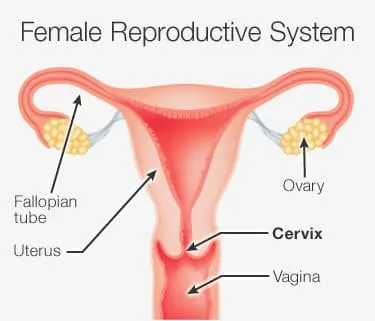
Determining the cause of cervicitis is important. If an infection is the problem, it can spread beyond the cervix to the uterus and fallopian tubes and into the pelvic and abdominal cavity and cause life-threatening infection. This may cause problems with fertility --the ability to become pregnant. Or it may cause problems with your unborn baby if you are already pregnant.
Here's what you need to know about symptoms, causes, risk factors, tests, diagnosis, and treatment of cervicitis.
What Is Cervicitis?
Cervicitis is inflammation of the cervix, which can be due to:
- Irritation
- Infection
- Injury of cells that line the cervix
These irritated or infected tissues may become red, swollen, and ooze mucus and pus. They may also bleed easily when touched.
What Causes Cervicitis?
Severe cases of inflammation are usually caused by infections that are passed during sexual activity.
Sexually transmitted diseases (STDs) that may cause cervicitis include:
- Gonorrhea
- Chlamydia
- Genital herpes
- Trichomoniasis
- Mycoplasma and ureaplasma
But many women with cervicitis don't test positive for any type of infection. Other causes of the inflammation may include:
- Allergies to chemicals in spermicides, douches, or to the latex rubber in condoms
- Irritation or injury from tampons, pessaries, or from birth control devices like diaphragms
- Bacterial imbalance; normal, healthy bacteria in the vagina are overwhelmed by unhealthy or harmful bacteria. This is also called bacterial vaginosis.
- Hormonal imbalance; having relatively low estrogen or high progesterone may interfere with the body's ability to maintain healthy cervical tissue.
- Cancer or cancer treatment; rarely, radiation therapy or cancer may cause changes to the cervix consistent with cervicitis.
Symptoms of Cervicitis
Many women with cervicitis don't have any symptoms. The condition may be discovered only after a routine exam or test.
Signs and symptoms, if present, may include:
- Grayish or pale yellow vaginal discharge
- Abnormal vaginal bleeding, such as bleeding after sex or between periods
- Pain during sex
- Difficult, painful, or frequent urination
- Pelvic or abdominal pain or fever, in rare cases
Risk Factors for Cervicitis
You may be at higher risk for cervicitis if you:
- Had recent sexual intercourse without a condom
- Recently had multiple sexual partners
- Have had cervicitis before
Studies show that cervicitis will recur in 8% to 25% of women who get it.
Diagnosing Cervicitis
If your doctor suspects you have cervicitis, they may do a pelvic exam. This lets the doctor get a closer look at the cervix.
The doctor will probably also swab the cervix to collect vaginal fluids or to see how easily it bleeds.
Your doctor will also probably ask questions about your sexual history. The doctor will want to know:
- The number of partners you've had in the past
- Whether or not you've had sex without a condom
- The kind of contraception you used
Even if you don't have symptoms, your doctor will perform a routine exam to look for cervicitis if:
- You are pregnant
- The doctor thinks you are at high risk for an STD
Tests for Cervicitis
Your doctor may swab the cervix to check for discharge, swelling, tenderness, and bleeding. Your doctor will test your vaginal fluid for the presence of harmful bacteria or viruses.
Cervicitis Treatment
You may not need treatment for cervicitis if a sexually transmitted infection is not the cause.
If an infection is suspected, the main goal of treatment is to eliminate the infection and prevent it from spreading to the uterus and fallopian tubes, or if you are pregnant, to your baby.
Depending on what organism is causing the infection, your doctor may prescribe:
- Antibiotics
- Antifungal medications
- Antiviral medications
Your doctor may also recommend that your partner be treated to make sure you don't get infected again. You should not have sex until you and your partner have finished treatment.
Treatment is especially important if you are HIV positive. That's because cervicitis increases the amount of virus that is shed from the cervix. This may increase your chances of infecting a partner. Also, having cervicitis can make it easier for you to get HIV from an HIV-positive partner.
If your symptoms persist despite treatment, you should be reevaluated by your doctor.
Nondrug treatments like douches or yogurt-based therapy do not work for cervicitis and may actually worsen symptoms. They are not recommended.
Preventing Cervicitis
You can decrease your risk of getting cervicitis by taking the following steps:
- Have your partner always use condoms during sex.
- Limit the number of people you have sex with.
- Don't have sex with a partner who has genital sores or penile discharge.
- If you get treatment for a sexually transmitted disease, ask your doctor if your partner should also be treated.
- Don't use feminine hygiene products. These may cause irritation of your vagina and cervix.
- If you have diabetes, try to maintain good control of your blood sugar.

